
Understanding Opioid Withdrawal Symptoms & Management: A Practical Guide to Safe Detox and Recovery
Opioid withdrawal is a mix of physical and emotional symptoms that happen when someone who’s developed dependence on opioids cuts back or stops. Without the right support it can be sudden, intense, and frightening. This guide lays out what withdrawal looks like, why symptoms occur, and which timelines and clinical approaches — including medically supervised detox and medication-assisted treatment (MAT) — improve safety and outcomes. Most people have both body symptoms (nausea, sweating, muscle aches) and mental-health challenges (anxiety, insomnia, cravings) that call for coordinated care. Understanding these patterns helps patients, families, and clinicians plan a safer detox and a clearer path into treatment. We map common symptoms, compare fentanyl timelines with other opioids, review evidence-based detox interventions, explain how inpatient rehab supports lasting recovery, offer family resources, and walk through insurance steps in Nevada. With symptom education plus practical next steps, readers can spot warning signs, seek supervised detox when needed, and activate supports that reduce risk and improve chances for recovery.
What Are the Common Symptoms of Opioid Withdrawal?
Opioid withdrawal typically follows a recognizable pattern of physical and psychological signs caused by a sudden drop in opioid receptor stimulation and the resulting autonomic rebound. In plain terms, when opioid signaling falls off, neurotransmitters and autonomic systems react — producing symptoms that range from uncomfortable to medically serious in vulnerable people. Spotting early versus later symptoms helps decide whether outpatient support is enough or if inpatient medical detox is needed. Clinicians commonly use tools like the COWS scale (Clinical Opiate Withdrawal Scale) to measure severity objectively. Below is a clear list of the most common physical and psychological signs, followed by a quick-reference table showing typical onset and expected course.
The list below summarizes top physical and psychological withdrawal signs with brief one-line definitions for quick reference:
- Nausea and vomiting: Stomach upset that can cause dehydration and electrolyte loss.
- Muscle aches and joint pain: Widespread soreness from autonomic rebound and inflammation.
- Sweating, chills, and gooseflesh: Overactive autonomic responses that affect body temperature.
- Runny nose, yawning, and watery eyes: Early autonomic symptoms that often signal the start.
- Insomnia and restlessness: Sleep disruption that worsens mood and mental focus.
- Anxiety, irritability, and mood swings: Emotional changes that raise relapse risk.
- Intense cravings: Strong urges to use opioids to relieve withdrawal distress.
- Diarrhea and abdominal cramping: Fluid losses that may require rehydration.
This quick table contrasts common symptom groups with typical onset and severity patterns to help guide monitoring and early intervention.
| Symptom Category | Typical Onset after Last Use | Typical Severity / Duration |
|---|---|---|
| Autonomic (sweating, chills, rhinorrhea) | 6–12 hours (short-acting opioids) | Peaks 24–72 hours; resolves days–weeks |
| Gastrointestinal (nausea, diarrhea) | 6–24 hours | Moderate-severe early; risk of dehydration |
| Musculoskeletal (aches, cramps) | 12–48 hours | Peaks 48–72 hours; improves over one week |
| Psychological (anxiety, insomnia, cravings) | 6–48 hours | Can persist weeks; protracted in some cases |
This comparison helps caregivers prioritize rehydration and close symptom monitoring while arranging psychological supports; changes in symptom type or intensity signal when medical supervision should be considered.
Which Physical Symptoms Indicate Opioid Withdrawal?
Physical withdrawal symptoms come from autonomic and gastrointestinal rebound and usually follow a predictable progression clinicians use to judge severity. Early signs often include yawning, watery eyes, runny nose, and sweating within hours of reduced opioid exposure. As withdrawal intensifies, nausea, vomiting, abdominal cramping, excess saliva, and profuse diarrhea can develop. Muscle aches, tremors, dilated pupils, and chills are common and may limit mobility, increasing fall and dehydration risk. Persistent vomiting or large fluid losses are red flags that need medical attention. Checking vital signs, tracking fluid balance, and using objective tools like the COWS scale help determine whether inpatient detox with IV fluids or medication support is needed to stabilize the person and prevent complications.
These physical signs naturally lead into the psychological side of withdrawal, which often adds to distress and shapes care decisions.
What Psychological Symptoms Accompany Opioid Withdrawal?
Psychological symptoms include anxiety, agitation, irritability, low mood, trouble concentrating, and intense cravings that may outlast the acute physical phase. These arise from shifts in brain chemistry — especially noradrenergic and dopaminergic systems — and can trigger suicidal thoughts or self-harm in people with pre-existing mood disorders, so prompt mental-health assessment is important. Non-drug coping tools such as paced breathing, predictable routines, supportive counseling, and brief behavioral strategies can lower acute distress and work alongside medications. Early connection to therapy, peer-support groups, and a clear post-detox psychosocial plan improves retention in treatment and reduces relapse risk. Often, the mix of psychological and physical symptoms determines whether inpatient care is the safest choice.
Understanding these mental-health impacts helps families and clinicians plan safety supports; next we’ll focus on fentanyl-specific timelines and risks.
How Does the Fentanyl Withdrawal Timeline Differ from Other Opioids?
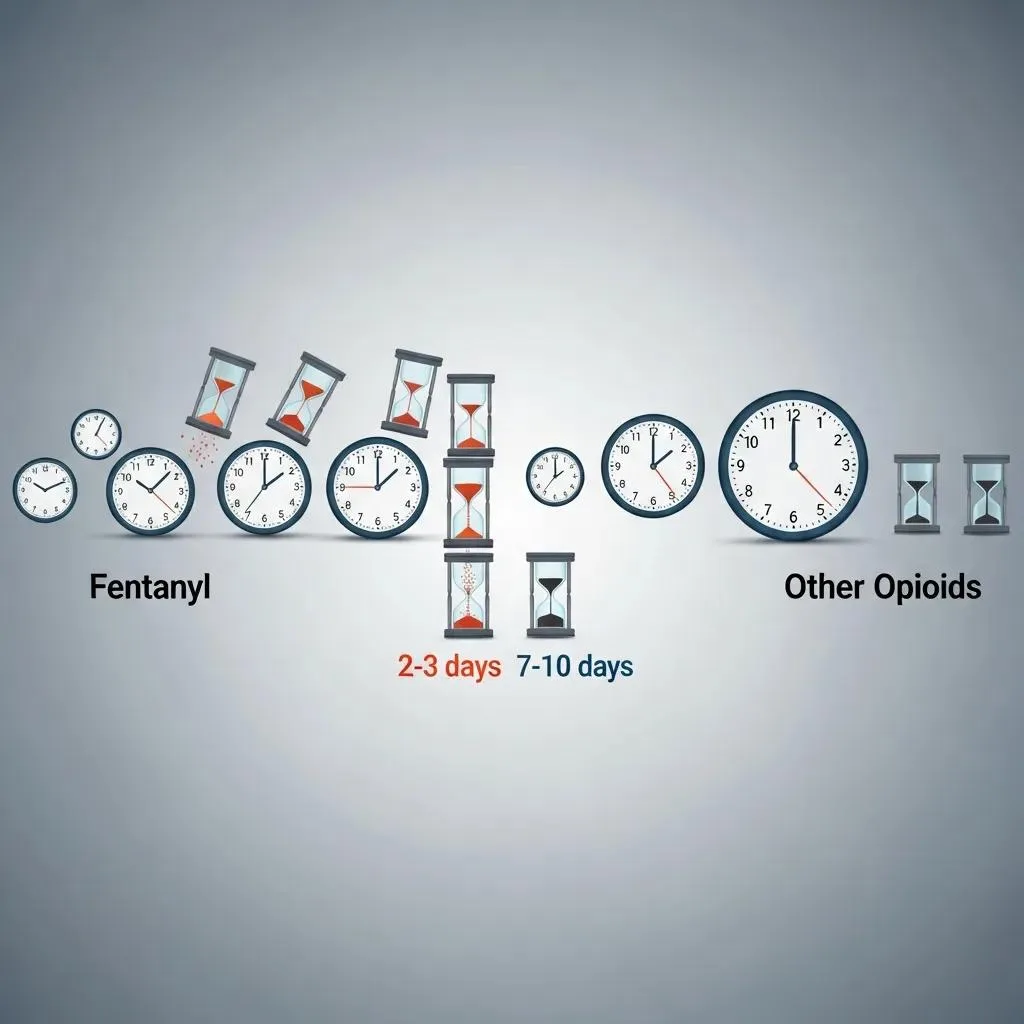
Fentanyl withdrawal can look different from other opioids because fentanyl is very potent, stores in fat tissue, and is often supplied in variable illicit forms. Those properties make onset and intensity more variable: fentanyl can build up in body fat and then redistribute unpredictably, producing abrupt neurochemical rebounds when blood levels drop. That may mean rapid, severe symptoms — and in some cases a longer or fluctuating course compared with heroin or prescription opioids. Clinically, this variability raises the stakes for medical supervision, since severe vomiting, dehydration, and cardiovascular issues can occur, and the high potency increases overdose risk if someone relapses. The brief timeline below compares onset, peak, and expected duration for fentanyl versus other opioid classes to help with triage and treatment planning.
Below is a three-line timeline-style comparison of onset, peak, and typical duration for fentanyl compared to heroin and methadone to illustrate these differences.
| Opioid Type | Typical Onset | Peak / Typical Duration |
|---|---|---|
| Fentanyl (illicit/potent) | 7–12 hours (can be unpredictable) | Peak 24–72 hours; symptoms may fluctuate and sometimes prolong for days–weeks |
| Heroin / short-acting prescription opioids | 6–12 hours | Peak 24–72 hours; most acute symptoms resolve in 5–7 days |
| Methadone (long-acting) | 24–48 hours | Peak 3–5 days; longer taper often required, symptoms may last weeks |
What Is the Onset and Duration of Fentanyl Withdrawal Symptoms?
Fentanyl withdrawal usually begins within hours of the last dose but can be unpredictable because of tissue redistribution; early signs may appear in 7–12 hours and often intensify over 24–72 hours. Peak physical discomfort — severe gastrointestinal losses, muscle pain, and autonomic instability — most commonly occurs in the first three days, while psychological symptoms and cravings can linger for weeks or recur later as protracted withdrawal. Factors that extend the timeline include high dose, frequent use, route of administration (transdermal vs. intravenous), co-occurring substance use, and individual metabolism. Those variables make personalized assessment and often longer monitoring necessary, especially after heavy or prolonged fentanyl exposure.
Recognizing fentanyl’s unique course helps explain why medical supervision is frequently the safest option.
Why Is Medically Supervised Detox Crucial for Fentanyl Withdrawal?
Medically supervised detox offers continuous vital-sign monitoring, rehydration, electrolyte correction, and targeted symptom medications to reduce the risk of serious complications from fentanyl withdrawal. Supervision aims to prevent dehydration from vomiting and diarrhea, lower the chance of arrhythmias from electrolyte imbalances, and provide immediate psychiatric support if severe anxiety or suicidal ideation emerges. Around-the-clock care allows rapid intervention when complications occur and supports timely initiation or continuation of MAT when appropriate. Given fentanyl’s potency and variable course, a supervised setting often provides safer stabilization than attempting withdrawal at home.
That safety focus leads into the evidence-based detox treatments and program elements used to manage withdrawal.
What Are Effective Medical Detox Treatments for Opioid Dependence?

Medical detox for opioid dependence is an evidence-informed process that stabilizes patients physically while beginning the transition to ongoing care. It combines medical monitoring, symptom-directed medications, hydration and nutrition support, and psychological care. The clinical goal is to replace or blunt withdrawal physiology and prevent complications, using short-term symptom medications and, when appropriate, starting MAT to reduce cravings and lower overdose risk. Effective programs use multidisciplinary teams — physicians, nurses, and therapists — to assess severity with tools like the COWS scale, individualize treatment, and create a discharge plan that links to counseling and community supports. Below are the core interventions you can expect during medical detox.
Medical detox typically includes these core interventions:
- Medical monitoring: Regular vital-sign checks and clinical assessments to catch complications early.
- Symptom-directed medications: Short-term drugs to ease nausea, diarrhea, insomnia, and anxiety.
- Rehydration and nutrition: IV or oral fluids and electrolyte replacement to treat losses from vomiting and diarrhea.
- Brief psychiatric support and safety planning: Crisis screening and initial mental-health stabilization when needed.
These interventions stabilize the patient and enable a safe transition to longer-term care, while preparing people for MAT or inpatient rehab when appropriate.
| Program Element | Typical Role | Expected Outcome |
|---|---|---|
| 24/7 medical monitoring | Ongoing assessment and rapid response | Reduced risk of medical complications |
| Symptom management medications | Targeted relief (antiemetics, antidiarrheals) | Improved comfort and retention in care |
| Hydration & electrolyte support | IV or oral replacement | Prevention of dehydration-related complications |
| Multidisciplinary team care | Integrated medical and behavioral supports | Better transition to ongoing treatment |
How Does Medical Detox at BetterChoice Treatment Center Support Safe Withdrawal?
At BetterChoice Treatment Center in Las Vegas, we provide medically supervised detox with a multidisciplinary clinical team — physicians, nurses, and therapists — available around the clock to manage withdrawal safely. Our approach pairs continuous monitoring and symptom-directed medical care with comfort-focused supports and optional holistic adjuncts such as yoga, sound therapy, and acupuncture to address both physical and emotional needs. Public listings show we work with major insurance providers and maintain regional accreditations, and our team coordinates care for co-occurring mental-health conditions. Intake typically includes a clinical assessment, benefits verification, and placement at the appropriate level of care so each person receives the right level of monitoring and support for their withdrawal severity.
This overview leads into the role of medication-assisted treatment as part of the care continuum.
What Role Does Medication-Assisted Treatment Play in Opioid Withdrawal Management?
Medication-assisted treatment (MAT) eases withdrawal and lowers cravings by using partial agonists or full agonists to stabilize opioid receptors, which reduces illicit opioid use and overdose risk. Common medications discussed in clinical practice include buprenorphine and methadone. By keeping receptors engaged in a controlled way, MAT prevents the abrupt neurochemical rebound that drives severe withdrawal and cravings and helps people participate in therapy and psychosocial care. MAT works best when paired with counseling, behavioral therapies, and discharge planning that support long-term recovery. At BetterChoice, we offer MAT options within a coordinated treatment plan under medical supervision — as one part of an individualized path forward, not a stand-alone fix.
With detox and MAT explained, the next section describes how inpatient rehab builds on stabilization to support lasting recovery.
How Does Inpatient Opioid Rehab Facilitate Lasting Recovery?
Inpatient opioid rehab offers a structured residential setting where people receive intensive therapy, medical oversight, peer support, and discharge planning designed to support sustained recovery. The model removes environmental triggers, provides predictable routines, and delivers evidence-based treatments to teach relapse-prevention skills. Typical program elements include daily individual therapy, group sessions, medication management, case coordination, and aftercare planning that connects patients to outpatient services or MAT maintenance. A controlled setting lets patients focus on therapeutic work — including building coping skills and addressing co-occurring mental-health disorders — which improves retention and prepares them for community-based recovery supports.
To clarify common therapeutic approaches used in inpatient programs, the list below explains core evidence-based therapies and their roles.
- Cognitive Behavioral Therapy (CBT): Teaches practical skills to change unhelpful thoughts and manage cravings.
- Motivational Interviewing (MI): Strengthens motivation to change and encourages engagement in treatment.
- Contingency Management: Uses positive reinforcement to support adherence to recovery goals.
What Evidence-Based Therapies Are Used in Inpatient Rehab?
Inpatient rehab commonly uses CBT, motivational interviewing, group therapy, and relapse-prevention training because these approaches produce measurable improvements in reducing opioid use and building coping skills. CBT helps restructure thinking and trains concrete techniques for managing cravings. MI boosts readiness for change and supports commitment to treatment plans. Group therapy creates peer support and shared learning, while relapse-prevention plans identify triggers, coping strategies, and emergency steps for cravings. These evidence-based methods are woven into a daily schedule so patients can practice skills in real time and build a clear plan for continued care after discharge.
How Do Holistic Therapies Aid Opioid Withdrawal and Recovery?
Holistic therapies — including yoga, acupuncture, mindfulness, and somatic practices — can reduce anxiety, improve sleep, and offer non-pharmacologic ways to manage pain and stress during withdrawal. These practices help down-regulate the stress response, support autonomic balance, and boost distress tolerance, making it easier to engage in therapy and reduce relapse triggers. Research supports their use as adjuncts (not replacements) for medical and behavioral treatments; when combined with clinical care they give people extra tools for emotional regulation and physical comfort during early recovery. Programs that blend holistic modalities with medical and psychotherapeutic interventions often report better patient satisfaction and stronger engagement with the overall plan.
Combining clinical and holistic strategies also helps families understand how to support their loved ones — the focus of the next section.
What Support Resources Are Available for Families of Individuals with Opioid Addiction?
Families are key to starting and sustaining recovery. They can help with safety planning, intake logistics, and family-focused therapy that addresses dynamics linked to substance use. Available supports include family counseling, educational sessions about withdrawal and relapse risk, community support groups, and state or national hotlines and referral services that connect families to local care. Preparing for intake — collecting medical history, insurance details, and a plan for transportation and care during early withdrawal — lowers barriers and increases the chance of timely admission. Below is a practical checklist families can use when preparing to help a loved one enter treatment, followed by resources to support family involvement during and after inpatient care.
The checklist below lists immediate steps families can take to prepare for intake and safe support.
- Gather medical and medication history: Include recent prescriptions and known allergies.
- Prepare basic identification and insurance information: Have policy numbers or member ID ready.
- Create a safety plan: List emergency contacts, remove substances from the home, and arrange supervision during early withdrawal.
How Can Families Help Loved Ones Navigate Opioid Withdrawal?
Families can help by encouraging medical supervision for withdrawal, assisting with transportation and intake logistics, and keeping a calm, nonjudgmental stance that prioritizes safety over confrontation. Bring a concise list of current medications, prior treatment records, and ID to intake, and be ready to share recent substance-use patterns to support clinical assessment. Communication tips: focus on immediate health and safety, avoid ultimatums that escalate conflict, and work with treatment staff to develop a realistic post-detox plan. Families should also watch for signs of severe withdrawal or suicide risk and seek emergency care if needed. These practical actions increase the chances of successful admission and protect the person during the high-risk early phase.
What Practical Resources Support Families During Treatment?
Families can tap national and state resources for education, referrals, and support groups; trusted sources like SAMHSA and NIDA offer guides and treatment locators to find local services. Family therapy and structured education programs address communication, boundary-setting, and relapse prevention, while peer-led groups give ongoing emotional support and shared problem-solving. Useful next steps include scheduling family therapy, joining local support meetings, and using vetted online materials to set expectations for recovery. Keeping family involvement within therapeutic channels improves outcomes and lowers the chance of enabling behaviors that undermine treatment.
How Can Patients Navigate Insurance for Opioid Addiction Treatment in Nevada?
Navigating insurance for addiction treatment follows a simple sequence: contact your insurer to confirm behavioral-health benefits, request any needed prior authorizations, and coordinate scheduling with the treatment provider to secure timely admission. Verification usually requires the member ID, service dates, and clinical justification (medical necessity); insurers often ask for clinical notes or documentation to support the requested level of care. Typical timelines — benefits checks within 24–72 hours and additional days for authorizations — help families plan and reduce delays. The table below summarizes common insurance steps, what to provide, and expected timelines so you can set realistic expectations.
The table below outlines the common insurance steps, what documentation to provide, and expected outcomes or timelines to set realistic expectations.
| Insurance Step | What to Provide | Expected Outcome / Timeline |
|---|---|---|
| Initial benefits check | Member ID, plan name, brief clinical summary | Confirmation of coverage within 24–72 hours |
| Pre-authorization request | Medical necessity documentation, treatment plan | Authorization decision in 3–7 business days (varies) |
| Scheduling & verification | Authorization numbers, provider details | Admission scheduled once authorization is confirmed |
What Steps Are Involved in Insurance Verification for Treatment?
Verification usually starts with a call to the insurer or the provider’s intake team to confirm whether addiction treatment is covered and which levels of care are authorized. Key documents are the insurance card or member ID, a short clinical summary (dates of use, previous treatments), and prescription records showing current medications — having these ready speeds the process. Ask specific questions about coverage for detox, inpatient rehab, MAT, and outpatient counseling, what prior-authorization rules apply, and whether there’s an appeals process for denials. Common delays come from missing documentation or waiting for physician notes; proactive coordination among family, clinician, and insurer reduces those barriers and speeds admission.
Which Major Insurance Providers Does BetterChoice Treatment Center Accept?
Public listings show BetterChoice Treatment Center accepts major insurance providers and that our admissions team works with payers to verify benefits and secure authorizations during intake to reduce financial uncertainty. Still, families should confirm plan-specific coverage and out-of-pocket costs directly with their insurer and ask admissions to run a benefits check before scheduling services. When verification is complete, request written authorization numbers and a clear summary of approved services (detox, inpatient, MAT) to avoid surprises at admission. Confirming these details ahead of time smooths entry into care and clarifies next steps for treatment planning.
If you need help right away, take these next steps: call a local treatment provider’s admissions team, request a benefits verification and any pre-authorizations, and have medical history and medication lists ready for clinical assessment. BetterChoice Treatment Center — a Las Vegas provider referenced in regional listings — offers multidisciplinary teams, 24/7 supervision, and holistic adjuncts as part of our detox and inpatient programs, and our admissions staff can assist with insurance verification and placement through our intake channels or public business listing. These steps shorten time to admission, match clinical needs to the right level of care, and help protect safety during the high-risk withdrawal period.
Frequently Asked Questions
What are the long-term effects of opioid withdrawal?
Long-term effects vary. Most physical symptoms ease within weeks, but psychological symptoms — anxiety, depression, and cravings — can persist for months or longer. Some people experience protracted withdrawal, where symptoms flare unpredictably. That’s why ongoing support, therapy, and a structured recovery plan are important to manage lingering effects and lower relapse risk.
How can I support someone going through opioid withdrawal?
Support means practical help and emotional steadiness. Encourage medical supervision when possible, listen without judgment, and help with logistics like transportation and appointments. Make the home environment safer by removing substances and triggers. Your steady presence and practical assistance can make a big difference in their chance of getting and staying in treatment.
What role does nutrition play during opioid withdrawal?
Nutrition matters. A balanced diet helps the body recover from the stress of withdrawal and can replace lost electrolytes and fluids after vomiting or diarrhea. Protein, vitamins, and minerals support healing and mood. Staying hydrated is essential — dehydration worsens symptoms. If possible, consult a healthcare provider or nutritionist for tailored guidance during withdrawal.
Are there alternative therapies that can help with opioid withdrawal?
Yes. Complementary practices like acupuncture, yoga, and mindfulness meditation can reduce anxiety, improve sleep, and support emotional balance during withdrawal. They’re useful adjuncts but not replacements for medical care. When combined with clinical treatment, these approaches can enhance comfort and overall well-being.
What should I expect during the first few days of opioid withdrawal?
Expect a range of symptoms that vary in intensity. Early signs often include anxiety, restlessness, muscle aches, and gastrointestinal upset. Symptoms commonly peak between 24 and 72 hours and can be distressing. Having a support system and, when possible, medical supervision helps manage symptoms and keeps the person safe during this critical window.
How can I find support groups for opioid addiction recovery?
Local treatment centers can point you to support groups like Narcotics Anonymous (NA) or SMART Recovery. Many communities offer in-person and virtual options. National resources such as SAMHSA and NIDA also provide directories and guidance to locate services near you. Peer support is a valuable part of recovery.
What are the signs that someone may need immediate medical attention during withdrawal?
Seek emergency care if you see severe dehydration (persistent vomiting or diarrhea), extreme agitation or confusion, suicidal thoughts, or signs of cardiovascular instability such as a very fast heartbeat or chest pain. If someone’s condition worsens or they’re in severe distress, prompt medical attention can prevent life-threatening complications.
Conclusion
Knowing the signs of opioid withdrawal and the options for safe management is essential to protect health and support recovery. Seeking medically supervised detox when appropriate, engaging MAT and therapy, and involving family supports all increase the chance of a successful outcome. If you or a loved one needs help, reach out to qualified providers, verify insurance benefits, and use the resources in this guide to take the next step toward recovery.
