
Medical Detox: What to Expect During Medically Supervised Withdrawal at BetterChoice Treatment Center
Medical detox is a supervised, clinical process for managing the physical and emotional symptoms that come when someone stops using drugs or alcohol. Its purpose is straightforward: reduce immediate risks, ease withdrawal where possible, and stabilize the person so they can safely move on to therapy and long-term care. This article walks through the detox process step by step — what it is, the stages you’ll likely see, common withdrawal symptoms by substance, and practical guidance for preparing and planning aftercare. We aim to ease uncertainty for people and families by outlining safety practices, typical timelines, and next steps, while emphasizing medically supervised care, medication-assisted options when appropriate, and smooth transitions into inpatient or outpatient programs. You’ll find clear lists and tables that compare withdrawal timelines and risks, summarize symptoms and management strategies, and match facility services to patient benefits to help with planning and conversations with loved ones or clinicians.
What Is Medical Detoxification and Why Is It Essential?
Medical detoxification is the controlled removal of substances under clinical supervision, combined with active monitoring and treatment of withdrawal symptoms to avoid complications and prepare the person for ongoing addiction care. It relies on regular clinical checks, symptom-focused medications when needed, and supportive nursing care to reduce physiological stress and lower the risk of serious events like seizures or delirium. The primary advantage is safety: supervised detox reduces the risk of harm during the acute withdrawal period and creates a stable starting point for counseling and rehabilitation. Current clinical guidance treats supervised detox as the first medical step in a larger continuum of care that should be followed by behavioral health treatment.
Medical detoxification delivers three practical benefits:
- Reduced risk: Ongoing monitoring and rapid medical response lower the chance of life‑threatening withdrawal complications.
- Better symptom control: Medication management and nursing support ease the intensity of withdrawal and increase comfort.
- Readiness for treatment: Stabilization makes it possible to start counseling, medication-assisted treatment, or longer-term rehab safely.
These benefits set the stage for the safety protocols used during medically supervised detox and explain how those measures protect patients in the acute phase.
How Does Medically Supervised Detox Ensure Safety and Comfort?
Safety in medically supervised detox comes from frequent vital-sign checks, structured clinical assessments, and immediate access to trained clinicians who can act quickly if problems arise. Typical monitoring includes scheduled checks of heart rate, blood pressure, temperature, breathing, and mental status to spot dehydration, autonomic instability, or severe agitation early. Symptom management can combine non-opioid and opioid medications when indicated, along with nursing care, hydration and nutrition support, and environmental adjustments to lower stimulation and anxiety. Comfort measures — such as targeted medications, restful accommodations, and short supportive interventions — help people get through the toughest hours while the care team focuses on stabilization. Clear documentation and open communication with the patient and family also support safety and preparation for the next step in treatment.
What Substances Are Commonly Treated During Medical Detox?
Medical detox most often treats withdrawal from alcohol, opioids (including prescription opioids and illicit fentanyl), benzodiazepines, and stimulants. Each class has a different timeline and risk profile. Alcohol and benzodiazepine withdrawal carry a higher risk of seizures and delirium tremens and commonly require close monitoring and tapering or symptom‑targeted medications. Opioid withdrawal is extremely uncomfortable, with flu‑like and autonomic symptoms, and may be managed with medication-assisted approaches to reduce cravings and physiological distress. Stimulant and cannabis withdrawal are usually treated with supportive care focused on psychological symptoms like anxiety and sleep problems. Knowing these differences helps clinicians set monitoring levels and lets patients and families know what to expect during the acute detox window.
What Are the Stages of the Medical Detox Process?
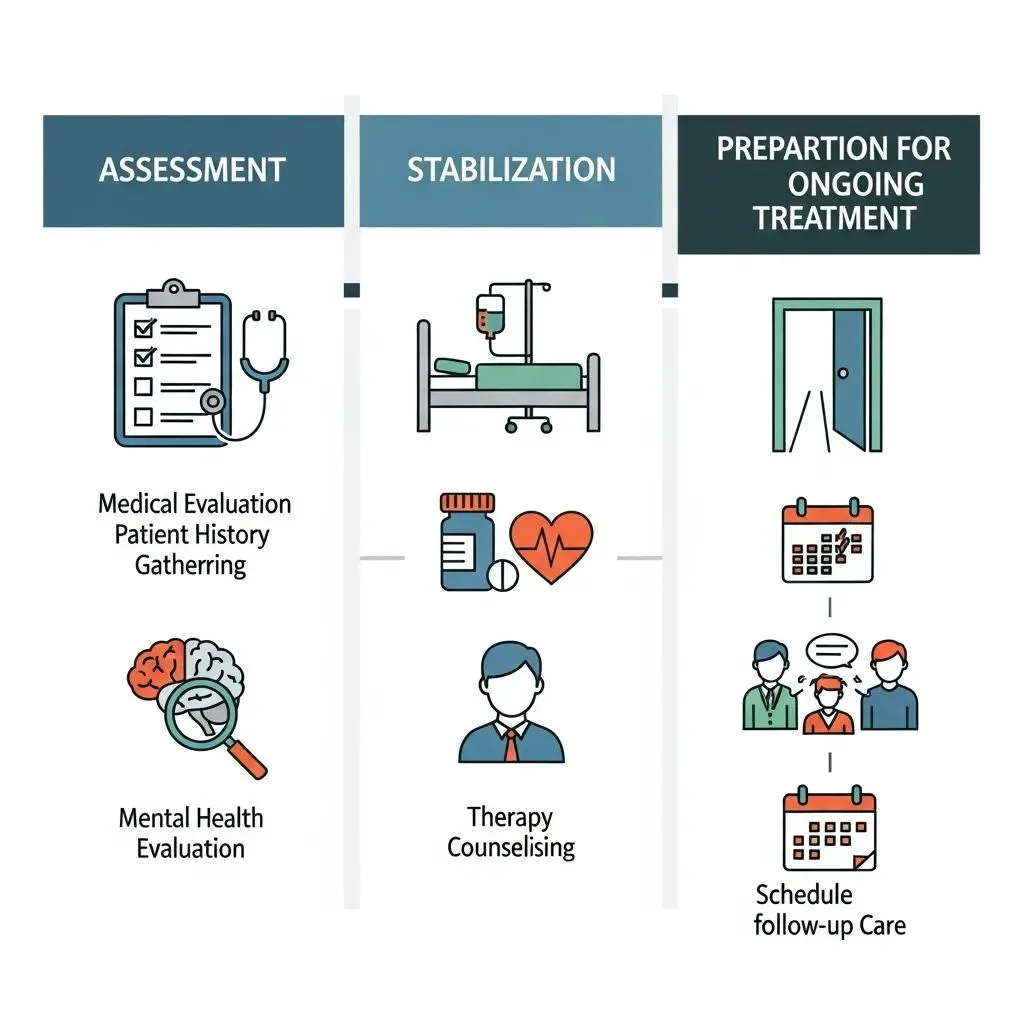
We typically describe medical detox in three stages: assessment and planning, acute withdrawal management and stabilization, and preparation for ongoing treatment and recovery. Each stage has a clear purpose—evaluation identifies risks and shapes an individualized plan; acute management handles immediate medical and emotional needs; and discharge planning connects the person to the next level of care. The ordered list below summarizes each stage so you know what to expect during a medically supervised detox episode.
- Stage 1: Initial assessment and personalized detox plan — A comprehensive intake gathers medical and substance-use history, screens for co-occurring conditions, and sets monitoring and medication strategies based on individual risk.
- Stage 2: Acute withdrawal management and stabilization — Increased observation, symptom‑directed medications, and nursing support are used during the peak withdrawal window to achieve clinical stability.
- Stage 3: Preparation for ongoing treatment and recovery — Discharge planning, referrals to inpatient or outpatient programs, and initiation of aftercare services create continuity after detox.
Stage 1: Initial Assessment and Personalized Detox Plan
The initial assessment establishes the care plan by collecting medical and psychiatric history, substance-use patterns, current medications, and details about social supports that affect safety and placement. Clinicians use this information to estimate risk and decide whether inpatient or outpatient observation is appropriate, plus how often to monitor and which symptom‑management strategies to use. Baseline labs and vital signs give reference points to track changes during withdrawal. Family or emergency contacts are recorded for communication, and insurance and intake logistics are handled to reduce delays. A clear, personalized plan helps match the level of supervision and clinical resources to each patient’s needs.
Stage 2: Acute Withdrawal Management and Stabilization
During acute withdrawal, staff step up observation to detect autonomic instability, severe agitation, or changes in mental status; the central aim is to keep the person physiologically stable while treating symptoms. Care typically includes scheduled vital‑sign checks, medication‑assisted strategies when clinically appropriate, fluid and electrolyte replacement, and trauma‑informed supportive care for anxiety and sleep problems. Monitoring often involves nursing checks every few hours and defined escalation criteria for deterioration; warning signs we watch for include rising heart rate, uncontrolled vomiting, altered mental status, and seizures. The table below compares common substances, typical withdrawal windows, and major risks so families can set realistic expectations about timing and severity.
| Substance | Typical withdrawal timeline & peak window | Key acute risks and symptom highlights |
|---|---|---|
| Alcohol | Onset 6–24 hours; peak 24–72 hours | Seizure risk, delirium tremens, autonomic instability, severe dehydration |
| Opioids | Onset 6–12 hours (short-acting) to 30 hours (long-acting); peak 24–72 hours | Intense autonomic symptoms, severe cramps, vomiting, risk of complications from comorbid illness |
| Benzodiazepines | Onset 1–7 days after reduction/cessation; peak varies | Protracted anxiety, severe seizure risk with abrupt cessation, confusion/delirium |
| Stimulants | Onset 12–72 hours; peak 24–72 hours | Severe fatigue, depression, acute agitation; lower risk for life-threatening physiological events |
Stage 3: Preparation for Ongoing Treatment and Recovery
Once someone is medically stable, the team focuses on discharge planning to ensure a safe handoff into continued care — whether that’s higher-intensity inpatient rehab, partial hospitalization, or outpatient services. Clinicians document a transition plan that includes follow-up appointments, prescriptions, and counseling referrals. Family involvement during this stage supports adherence to aftercare and helps set expectations about visits and communication. Practical checklists — covering transportation, post‑discharge medications, and scheduled therapy — reduce gaps that can lead to early relapse. Completing Stage 3 results in an actionable continuity‑of‑care plan linking detox to longer‑term recovery supports.
What Withdrawal Symptoms Can You Expect During Detox?

Withdrawal symptoms can be physical, emotional, or both, and they vary by substance, dependence severity, and overall health. Care teams prioritize early detection and targeted treatment. Physical signs often include tremor, sweating, and gastrointestinal upset; emotional symptoms can range from anxiety and depression to intense cravings. Management strategies include close monitoring, symptomatic medications, behavioral support, and environmental steps that reduce stimulation and promote rest. The list below highlights major symptoms and the substances where they commonly occur so families know what to anticipate.
- Autonomic and motor symptoms: Tremor, sweating, fast heart rate — commonly seen with alcohol and benzodiazepines.
- Gastrointestinal symptoms: Nausea, vomiting, diarrhea, abdominal cramps — prominent in opioid withdrawal.
- Sleep and mood disturbances: Insomnia, anxiety, low mood, strong cravings — frequent across multiple substances.
- Severe neurologic risks: Seizures and delirium — highest risk after abrupt alcohol or benzodiazepine cessation.
What Are Common Physical Withdrawal Symptoms by Substance?
Physical withdrawal signs differ by substance and timing, and clinicians use those patterns to guide monitoring. Alcohol and benzodiazepine withdrawal can cause tremors, heavy sweating, high blood pressure, and seizures, often appearing within the first day and peaking over 24–72 hours — which is why these cases usually need the most medical oversight. Opioid withdrawal typically brings muscle aches, stomach upset, gooseflesh, and autonomic overactivity that peak around 24–72 hours for many drugs and are managed mainly for comfort and safety. Stimulant withdrawal often causes deep fatigue, excessive sleepiness, and general malaise without the same seizure risk, while cannabis withdrawal tends to cause irritability, sleep problems, and appetite changes. The table below summarizes symptom categories, typical features, and common management approaches.
| Symptom category | Physical / Psychological | Examples + management strategies |
|---|---|---|
| Tremor & autonomic | Physical | Tremor, tachycardia, hypertension — managed with monitoring, hydration, and targeted medication when indicated |
| Gastrointestinal | Physical | Nausea, vomiting, diarrhea — managed with antiemetics, rehydration, and electrolyte replacement |
| Sleep disturbance | Psychological/physical | Insomnia, hypersomnolence — managed with sleep hygiene, short-term pharmacotherapy if clinically appropriate |
| Seizure risk | Physical (high-risk) | Seizures, severe agitation — escalation to higher-level care and seizure prophylaxis/treatment when indicated |
What Psychological Symptoms May Occur and How Are They Managed?
Psychological symptoms during detox often include anxiety, irritability, low mood, agitation, panic, and strong cravings that may continue after physical symptoms ease and complicate early recovery. Care focuses on ongoing psychiatric assessment, supportive counseling, relapse‑prevention coaching, and, when appropriate, short‑term medication strategies that avoid highly addictive agents. Low‑stimulation rooms, predictable daily routines, and brief therapeutic support help reduce agitation and improve sleep. Early screening for co‑occurring mental health conditions guides referrals to specialized care. Families and clinical teams should expect that psychological symptoms may require longer‑term therapy beyond the detox stay and that connecting to outpatient mental health services improves chances for sustained recovery.
How Does BetterChoice Treatment Center Support You Through Detox?
At BetterChoice Treatment Center in Las Vegas, we provide medically supervised detox and inpatient rehab with a model built around continuous clinical oversight and coordinated transitions to ongoing care. Our multidisciplinary approach — led by medical leadership and experienced clinical staff — follows recognized quality standards such as LegitScript and The Joint Commission Gold Seal of Approval. Core features include 24/7 supervision, medication management, psychosocial supports, and optional complementary therapies to improve comfort during the acute phase. The table below links specific services to what they deliver and how patients benefit, presented as a factual overview of facility supports.
The following table outlines core services and practical benefits patients can expect during medically supervised detox at the facility, linking service features to clinical implementation and patient outcomes.
| Service / Feature | What it provides | Patient benefit + implementation detail |
|---|---|---|
| 24/7 medical supervision | Continuous nursing and physician oversight | Rapid response to complications; structured monitoring protocols to maintain safety |
| Multidisciplinary team | Medical director, clinical staff, therapists | Integrated care decisions and coordinated treatment planning under clinical leadership (named leadership included) |
| Holistic therapies & amenities | Supportive non-clinical therapies | Adjunctive comfort and stress reduction integrated with medical care to improve tolerability |
| Insurance and care coordination | Assistance with placement and verification | Practical help arranging next-level care and addressing authorization needs for continuity |
Who Are the Medical Experts Providing 24/7 Supervision?
Clinical oversight during medically supervised detox typically includes a medical director who sets clinical protocols, nursing staff who perform continuous monitoring and medication administration, and behavioral health clinicians who provide counseling and discharge planning. At the facility level, named clinical leadership roles — such as Medical Director, Clinical Director, Quality Assurance, and CADC‑I — contribute to assessment, safety planning, and coordinated care. Physicians and nurse practitioners make medication decisions; registered nurses monitor vitals and deliver treatments; and counselors offer psychosocial support and family communication. This multidisciplinary team ensures that medical, behavioral, and quality perspectives guide stabilization and transition planning.
What Luxurious Amenities and Holistic Therapies Enhance Comfort?
Comfort-focused supports can include quiet private rooms, structured rest periods, and optional holistic therapies like relaxation exercises, guided breathing, gentle movement classes, or acupuncture when available. These services are adjuncts to medical care — they reduce stress, support sleep, and teach coping strategies for anxiety and cravings without replacing evidence‑based medical interventions. Amenities that prioritize rest, hydration, and nutrition help patients preserve strength during withdrawal and make the stay more tolerable. Presenting these options as complementary helps families understand their role in comfort and recovery while clinical teams focus on medical stabilization.
How Should Patients and Families Prepare for the Medical Detox Journey?
Getting ready for medical detox helps speed intake and improves safety and placement by gathering key documents and planning logistics. Recommended preparation includes bringing government ID, insurance details, a current medication list with doses and prescribers, recent lab records if available, and emergency contact information. Families should also plan transportation, storage for personal items, and emotional preparation by setting boundaries and learning supportive communication strategies. The checklist below lists concrete pre‑arrival steps that make intake smoother and protect patient safety.
- Gather identification and insurance information: Bring a valid ID and insurance details to speed verification and placement.
- Prepare a current medication list: Document prescription and over-the-counter medications, doses, and prescriber names for reconciliation.
- Pack essential personal items: Bring comfortable clothing, necessary toiletries, and any required medical devices; leave valuables at home.
- Arrange logistics and contacts: Plan transportation, designate an emergency contact, and inform family members about expected visitation policies.
What Steps Should Patients Take Before Arrival?
Before arrival, patients should share a full medication and substance‑use history, disclose medical conditions and allergies, and bring recent medical records when possible so clinicians can assess risk and make informed medication choices. Completing pre‑admission paperwork and verifying ID and insurance ahead of time can shorten wait times and let the team begin the personalized plan faster. Practically, patients should not bring illicit substances or contraband and should be ready for a medically supervised environment with structured routines. Honest communication about past detox experiences or adverse events such as prior seizures helps the clinical team set the right monitoring level and prevent avoidable complications. These steps improve safety and speed a timely start to detox care.
How Can Families Support Loved Ones During Detox?
Families can help by offering calm emotional support, using nonjudgmental language, and taking care of practical tasks like transportation and personal affairs while their loved one is in care. It’s important to respect privacy and consent rules — clinical staff will explain visitation and communication policies and involve family members as appropriate in discharge planning. Useful family actions include joining care coordination meetings, learning about aftercare options, and avoiding enabling behaviors that undermine treatment goals. Thoughtful family involvement during discharge planning improves continuity of care by helping secure housing, transportation, and follow-up appointments for the person leaving detox.
What Comes After Detox? Transitioning to Inpatient and Outpatient Rehab
Detox treats physical dependence but does not address the behavioral, psychological, and social drivers of substance use. Continued care is essential to lower relapse risk and address underlying issues. Typical next steps include inpatient rehabilitation, partial hospitalization, intensive outpatient programs, and outpatient counseling; medication‑assisted treatment is also an option for opioid and alcohol use disorders when clinically appropriate. Care coordination during the transition focuses on assessing needs, arranging placement, and scheduling intake for the next level of care to minimize gaps between discharge and ongoing treatment. The stepwise flow below shows common transition steps used to keep clinical momentum and support longer‑term recovery.
- Assessment for placement: Clinicians evaluate clinical stability and treatment needs to recommend inpatient or outpatient options.
- Placement and authorization: Care coordinators verify insurance and arrange admission to the selected program or schedule outpatient follow-up.
- Handoff and follow-up scheduling: Medical summaries, prescriptions, and appointments are provided to ensure continuity and adherence.
Why Is Continued Care Critical for Lasting Recovery?
Detox addresses physiological dependence but not the learned behaviors, coping gaps, and social factors that contribute to substance use. Ongoing therapy, peer supports, and medication‑assisted treatment where indicated are proven to improve long‑term outcomes compared with detox alone. Continued care lets people address co‑occurring mental health conditions, practice relapse‑prevention skills, build sober supports, and receive ongoing monitoring. Planning for and engaging in aftercare is one of the strongest predictors of whether detox leads to sustained recovery.
How Does BetterChoice Facilitate a Smooth Transition to Rehab Programs?
BetterChoice helps coordinate transitions by completing placement assessments, verifying coverage, and arranging referrals to appropriate inpatient or outpatient programs to maintain continuity after detox. Our care coordination pathway generally follows a clear process: assessment → placement recommendation → authorization and scheduling → handoff to the receiving program with clinical summaries and follow‑up instructions. Patients and families are encouraged to contact the facility with questions about insurance or placement preferences; neutral next steps include calling the facility phone number or discussing local placement options with clinical staff. By documenting and communicating each step, our care coordinators work to reduce service gaps and promote timely engagement in ongoing treatment.
This completes the content under the last provided heading.
Frequently Asked Questions
What is the role of family during the detox process?
Family support plays an important role during detox. Loved ones can provide emotional reassurance, help with transportation and practical matters, and participate in care meetings when appropriate. It’s important for family members to respect privacy and consent rules; clinical staff will explain visitation policies and involve family in discharge planning as allowed. Active, informed family participation can strengthen continuity of care by helping arrange housing, transportation, and follow-up appointments after detox.
How long does the medical detox process typically take?
Detox length varies by substance, severity of dependence, and individual health. Generally, detox lasts from a few days up to a couple of weeks. Alcohol and benzodiazepine detoxes may take longer because of higher seizure risk and the need for careful tapering, while opioid detox is often shorter. Individualized monitoring and treatment plans determine the appropriate length of stay to ensure safety and effective symptom management.
What happens if a patient experiences a relapse during detox?
If a relapse occurs during detox, the clinical team will assess the situation immediately and adjust care as needed. Responses may include changing medications, increasing monitoring, or providing extra psychological support. The priority is to stabilize the person and keep them safe while addressing the factors that led to the relapse. Open communication with the patient and family supports a prompt, appropriate response.
Are there any specific dietary recommendations during detox?
Nutrition and hydration matter during detox. A balanced diet rich in vitamins and minerals supports recovery, and staying hydrated helps manage many withdrawal symptoms. Facilities typically provide nutritious meals tailored to individual needs, and consulting with a nutritionist can be helpful for personalized guidance. Proper nutrition supports healing and helps reduce some physical symptoms of withdrawal.
What types of therapies are available during detox?
Detox often includes a mix of medical care and supportive therapies. Holistic options such as yoga, meditation, and acupuncture may be available to reduce stress and promote relaxation. Behavioral therapies like cognitive‑behavioral therapy (CBT) can help address psychological symptoms and teach coping skills. These therapies complement medical treatment to improve comfort and prepare patients for continued care after detox.
How can patients ensure a successful transition to aftercare?
To increase the chances of a smooth transition, patients should take an active role in discharge planning, follow clinical recommendations, attend follow-up appointments, take prescribed medications as directed, and engage in outpatient therapy or support groups. Building a strong support network of family, friends, and peers also helps. Honest communication with the care team about needs and challenges during the transition period is essential for sustained recovery.
Conclusion
Knowing what to expect from medical detox can reduce anxiety and help people and families make informed decisions. Medically supervised detox provides safety, symptom relief, and a stable starting point for ongoing treatment — all key steps on the path to recovery. With preparation, family support, and a clear plan for aftercare, individuals can move through detox with greater confidence and connect to the services they need next. For more information about beginning your recovery journey, explore our resources or contact our team.
