
Opioid Detox Program — Summerlin, Nevada: A Clear, Safe Path to Recovery
Medically supervised opioid detox helps people safely manage withdrawal from opioids — including prescription pain medicines, heroin, and fentanyl — and is often the first step toward lasting recovery for many Summerlin residents. This guide explains opioid use disorder, why supervised detox improves safety and stabilization, how a clinical detox program typically runs, what withdrawal symptoms and timelines usually look like, and practical next steps for families and payers. You’ll find clear explanations of detox phases, common medications and monitoring approaches, expected symptom patterns by opioid type, and how families and insurance fit into admissions and aftercare planning. Throughout, we rely on evidence-based practice, explain the clinical reasons for supervised care, and give Summerlin residents concrete actions to take when seeking help.
What Is Opioid Addiction and Why Is Detox Essential in Summerlin?
Opioid addiction — clinically called opioid use disorder — is a chronic medical condition marked by compulsive opioid use despite harm. Repeated opioid exposure changes brain reward systems and breathing control, which drives strong cravings and raises the risk of life-threatening respiratory depression with misuse. Medically supervised detox gives continuous clinical observation, symptom relief, and emergency response capacity that lower the chance of complications such as severe dehydration, uncontrolled anxiety, or accidental overdose after a period of reduced tolerance. For people in Summerlin, local access to supervised detox means faster assessment and a safer bridge to ongoing treatment. The section that follows explains common opioids and how each affects the body so families and clinicians can anticipate different withdrawal needs.
Key reasons supervised detox is recommended for safety and better outcomes:
- Continuous medical monitoring reduces the chance of unmanaged complications during withdrawal.
- Medication-assisted approaches lessen withdrawal intensity and support stabilization.
- Care teams create individualized plans to transition patients to inpatient or outpatient treatment.
These points summarize why clinical supervision matters and lead into a closer look at specific opioids and their effects.
What Are Common Opioids and Their Effects on the Body?
Common opioids include prescription pain relievers (for example, oxycodone and hydrocodone), heroin, and synthetics like fentanyl. All opioids bind receptors that reduce pain and produce sedation; short-term effects can include pain relief, euphoria, slowed breathing, and constipation. Over time, tolerance and physical dependence develop, and hormonal and respiratory regulation can be altered — raising overdose risk. Illicit heroin and fentanyl are especially risky because potency and contamination can be unpredictable; fentanyl’s high strength can deepen dependence and change withdrawal timing. Knowing these substance-specific differences explains why clinicians tailor monitoring and medications during detox and helps families expect different withdrawal patterns.
Why Is Medically Supervised Detox Crucial for Opioid Withdrawal?
Unsupervised withdrawal can lead to dehydration, unstable vital signs, and a higher risk of relapse or accidental overdose once tolerance drops, so medically supervised detox prioritizes safety. In a supervised setting you get regular vital checks, hydration and nutrition support, symptom-targeted medications, and 24/7 nursing capable of responding to respiratory or cardiovascular emergencies. Clinical programs also offer Medication-Assisted Treatment (MAT) and monitored tapers, which reduce symptom severity and allow for a planned transition to longer-term care. Choosing supervised detox improves immediate safety and creates opportunities to start evidence-based follow-up treatment, helping close gaps that often trigger relapse. These safety measures set the stage for a clear description of a typical detox workflow: intake, stabilization, medication management, and transition planning.
How Does the Opioid Detox Process Work at BetterChoice in Summerlin?

At BetterChoice, medically supervised opioid detox follows a consistent clinical flow: intake and assessment, stabilization with symptom control, medication management or tapering when appropriate, and discharge with a clear plan for ongoing care. Intake includes a clinician-led medical and psychiatric review, vital signs, and baseline labs to identify co-occurring conditions and set monitoring needs. Stabilization involves frequent nursing checks, symptom-directed medications, hydration and nutrition support, and evaluation for MAT when indicated. Transition planning connects patients with inpatient rehab, outpatient programs, counseling, or other services to reduce relapse risk and support recovery. Below is a step-by-step outline that links each phase to its clinical purpose and daily activities so patients and families know what to expect when entering detox in Summerlin.
The core detox steps, for quick reference:
- Intake and clinical assessment to document medical history and establish baseline vitals.
- Stabilization with 24/7 nursing, symptom control, and initial medication decisions.
- Medication-assisted management or tapering under physician supervision.
- Discharge planning that arranges inpatient or outpatient transition and aftercare supports.
This stepwise overview clarifies the patient journey and leads to a concise table describing each phase and typical clinical actions.
Introductory table describing each detox phase, its purpose, and typical clinical actions:
| Detox Step | Medical Purpose | Typical Actions/Monitoring |
|---|---|---|
| Intake & Assessment | Identify medical and psychiatric risks and establish baseline status | Medical history review, vital signs, labs, substance screening, mental health evaluation |
| Stabilization | Control acute withdrawal symptoms and prevent complications | Frequent vitals, IV fluids if needed, symptomatic medications, close nursing observation |
| Medication Management/Taper | Reduce withdrawal severity and prepare for MAT or safe discontinuation | Buprenorphine or taper plans as appropriate, medication monitoring, naloxone education |
| Transition & Aftercare Planning | Ensure continuity of care and reduce relapse risk | Referrals to inpatient/outpatient programs, scheduling counseling, family planning |
This table clarifies daily expectations during detox and supports informed decision-making before admission.
What Is the Step-by-Step Medical Detox Program for Opioids?
Day one starts with a focused clinical intake documenting opioid type, last use, medical history, and current symptoms to guide immediate safety steps and medication choices. During the first 48–72 hours clinicians prioritize stabilization with frequent vital checks, symptom scoring, hydration, and targeted medications (for example, clonidine for autonomic symptoms or antiemetics for nausea). Nursing staff watch for signs of severe withdrawal or complications. While stabilizing, providers assess eligibility for MAT — including buprenorphine — and plan a safe initiation when appropriate. Discharge planning begins early so the team can arrange next-level care (inpatient rehab or outpatient services) and provide naloxone and overdose-prevention education before discharge. These daily milestones describe what patients and families can expect and lead into the medication options used in opioid and fentanyl detox.
Which Medications Are Used in Opioid and Fentanyl Detox?
Medication choices are individualized but commonly include buprenorphine (a partial opioid agonist) for tapering or maintenance, clonidine for autonomic symptom relief, antiemetics and antidiarrheals for symptom control, and naloxone as the emergency reversal agent in case of overdose. Buprenorphine reduces cravings and withdrawal intensity through partial receptor agonism, making it central to many MAT plans; clonidine helps blunt sympathetic symptoms like sweating and rapid heart rate without being an opioid. Clinicians monitor for drug interactions and adjust doses based on withdrawal severity, other medications, and co-occurring health issues. Education about naloxone distribution and overdose prevention is standard so patients and families know how to respond after discharge. This medication overview prepares readers for symptom timelines and decisions about longer-term treatment.
What Are the Symptoms and Timeline of Opiate Withdrawal in Summerlin?
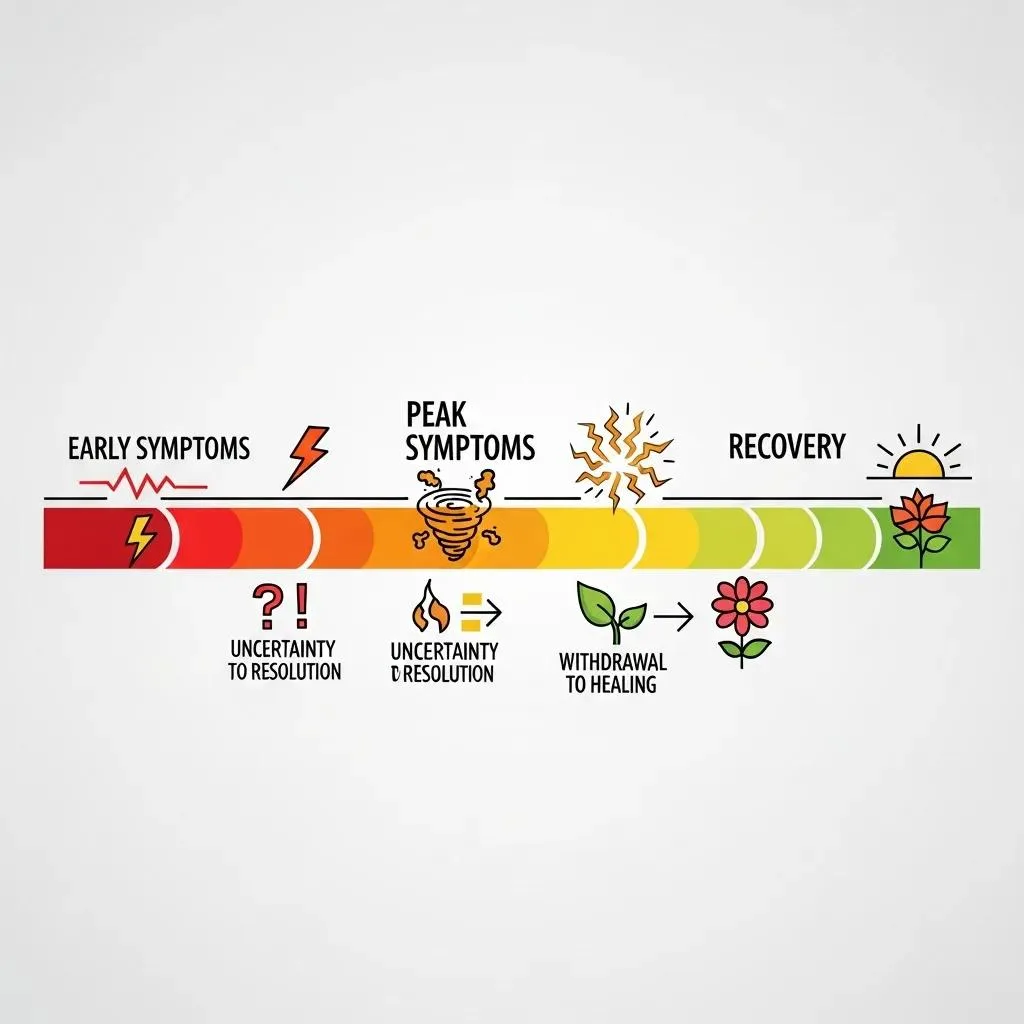
Opioid withdrawal commonly moves from an early phase of anxiety and GI upset to a peak of severe flu-like symptoms, then into a subacute recovery period that can include sleep and mood disturbances. Exact timing depends on opioid type, dose, and duration of use. Short-acting opioids often cause early symptoms within 6–12 hours, while peak symptoms usually occur on days 2–4 and include muscle aches, nausea, vomiting, and insomnia. Fentanyl and other high-potency synthetics can make the course longer or more intense and may require extended monitoring and MAT. Proper symptom management, hydration, and medical oversight lower acute risks and support a smoother transition to ongoing care. The table below compares typical onset and peak days for common opioids to help set expectations.
This short comparative table helps clinicians, patients, and families anticipate symptom timing for different opioids.
| Opioid Type | Typical Onset | Common Symptoms & Peak Days |
|---|---|---|
| Heroin | 6–12 hours after last use | Early yawning and anxiety; peak muscle aches and GI upset on days 2–4 |
| Prescription short-acting opioids | 8–24 hours | Nausea, sweating, insomnia; peak around days 2–4 |
| Fentanyl (synthetic) | 12–36 hours (variable) | Intense, sometimes prolonged symptoms; peak may extend to days 3–6 with longer subacute effects |
This timeline sets realistic expectations and reinforces why monitoring and individualized care are important during detox.
What Are Common Opioid Withdrawal Symptoms to Expect?
Common withdrawal symptoms include gastrointestinal distress (nausea, vomiting, diarrhea), muscle and joint aches, sweating and chills, faster heart rate and higher blood pressure, anxiety, and strong cravings. Psychological effects such as irritability, insomnia, and low mood are also common. The pattern typically starts with autonomic signs — yawning, tearing, runny nose — and progresses to more intense body aches and GI symptoms in the first few days. While withdrawal is rarely directly fatal, dehydration, electrolyte problems, and co-occurring medical issues can raise risk, which is why supervised detox focuses on fluids and symptom management. Knowing the common symptoms helps patients and families prepare and plan for aftercare.
Quick checklist of typical withdrawal symptoms:
- Nausea and vomiting
- Muscle aches and cramps
- Sweating and chills
- Anxiety, insomnia, and cravings
This checklist clarifies what to expect and leads into specifics about fentanyl-related timelines and why they sometimes require extended monitoring.
How Long Does Fentanyl Detox Typically Take?
Fentanyl detox timelines vary because fentanyl’s potency and pharmacology can create deeper dependence and a potentially longer withdrawal course. Acute symptoms often begin within 12–36 hours and may peak around days 3–6; post-acute symptoms can linger for weeks in some people. Factors that lengthen detox include higher doses, longer use, polysubstance patterns, and individual metabolism, which is why clinicians frequently recommend careful assessment and early consideration of MAT rather than abrupt cessation. Given fentanyl’s potency, teams commonly use a conservative, monitored approach with medication support and extended transition planning to reduce relapse and overdose risk after tolerance falls. Knowing this variability sets expectations for a tailored treatment plan and follow-up care beyond the acute withdrawal window.
In short: fentanyl withdrawal often requires more intensive monitoring and individualized medication planning than withdrawal from shorter-acting prescription opioids, which informs stabilization, MAT, and aftercare decisions.
Why Choose BetterChoice Treatment Center for Opioid Detox in Summerlin?
BetterChoice Treatment Center delivers medically supervised detox in the Summerlin area with a clinical model built around safety, stabilization, and smooth transitions to higher levels of care when needed. Our multidisciplinary approach combines medical oversight, nursing care, counseling, and discharge planning so patients move from detox into ongoing treatment with support. BetterChoice’s licensure and recognized accreditations provide verifiable trust signals families can use when comparing local options. The sections below describe our clinical roles, accreditations, and the complementary amenities and therapies that support comfort during detox while keeping medical care front and center.
Clinical and program features patients typically encounter:
- Medical director and clinical leadership coordinating individualized care plans
- 24/7 nursing and monitoring during stabilization
- Integrated counseling and referral pathways to inpatient or outpatient programs
These highlights preview facility details and prepare readers for information about accreditation and supportive services.
What Accredited and Expert Care Does BetterChoice Provide?
BetterChoice lists named clinical and administrative contacts and maintains licensure and accreditation consistent with safe medical detox operations. We note verification from Nevada’s Health Workforce, LegitScript, and The Joint Commission as indicators of adherence to recognized clinical standards. Our care team typically includes a medical director, clinical leadership, nursing staff, and counselors who work together to assess medical needs, manage medications, and arrange transitions to ongoing care. Presenting these facts helps families evaluate the structure of care and supports informed conversations with admissions staff about clinical capabilities and safety protocols.
This factual description supports decision-making and leads into a discussion of amenities and holistic supports that can complement medical treatment.
How Do Luxury Amenities and Holistic Therapies Support Recovery?
Comfort-focused amenities and adjunctive holistic therapies — like guided relaxation, sleep-supportive routines, and evidence-informed stress-reduction activities — can reduce distress during detox and improve engagement with clinical care. These offerings do not replace medical treatment but help lower anxiety, improve rest, and provide coping tools that make counseling and recovery activities easier to use. Examples include guided relaxation, gentle movement classes, and structured peer support sessions that promote emotional regulation and resilience. Framing these adjuncts as part of an integrated plan makes it clear they enhance, rather than substitute for, evidence-based medical detox and aftercare.
This perspective emphasizes that holistic measures complement medical care to support a comfortable, clinically guided recovery experience.
How Can Families Support Loved Ones During Opioid Detox in Summerlin?
Families are central to the recovery process by preparing logistics, offering steady emotional support, and coordinating with clinical teams to create a safer post-detox environment. Practical steps include gathering medical history and current medication lists before intake, arranging transportation and personal items, and planning to join family education or therapy sessions during discharge planning. Family members should also learn about overdose prevention — including naloxone use and safer post-detox monitoring — because lowered tolerance increases overdose risk after abstinence. The list below highlights concrete, compassionate actions families can take before, during, and after detox to support recovery while respecting the patient’s autonomy and clinical guidance.
- Gather medical records, current medication lists, and recent prescription information.
- Coordinate transportation and personal logistics for admission and discharge.
- Participate in family education or planning sessions to support continuity of care.
These steps provide a practical structure for family involvement and lead into available family therapy resources through the treatment team.
What Family Therapy and Resources Are Available at BetterChoice?
BetterChoice arranges family education sessions, counseling referrals, and participation in discharge planning to support understanding and long-term relapse prevention. Families may be invited to clinically supervised meetings, brief counseling to align expectations, and education about withdrawal and relapse risks. Staff provide guidance on supporting medication adherence and aftercare appointments while protecting patient confidentiality and timing family involvement to the patient’s readiness. These resources are practical supports aimed at helping families play a positive role in recovery; admissions staff can arrange participation and answer questions about how family services work.
This description prepares families for ways they can help and leads into evidence-based reasons why family involvement improves outcomes.
How Does Family Involvement Improve Recovery Outcomes?
Family involvement strengthens recovery by offering social support, helping maintain treatment adherence, and creating a safer home plan after discharge. Supportive family engagement reduces isolation, reinforces medication schedules and follow-up appointments, and helps implement environmental safeguards such as removing unsecured medications. Clinically, family-centered planning encourages accountability and continuity of care, which correlate with better engagement in outpatient or inpatient follow-up. Families who learn about addiction as a medical condition and practice communication strategies can reduce conflict and increase the chances of sustained treatment participation, supporting long-term recovery.
These evidence-aligned reasons explain why family engagement is an important part of the detox-to-recovery pathway.
What Are the Costs and Insurance Options for Opioid Detox in Summerlin?
Costs and coverage for detox services vary widely by payer, plan, and clinical need, so verifying benefits with both your insurer and the treatment provider is a crucial first step. BetterChoice lists several insurers commonly accepted, but listing does not guarantee coverage — pre-authorization, medical necessity documentation, and plan-specific rules are typical. If private pay or immediate admission is needed, discuss payment options with admissions to clarify rates and required documentation. The table below summarizes payment types, common coverage characteristics, and concrete actions families can take to verify benefits and prepare for admission.
Before using the table, gather your insurance card, recent prescription history, and a summary of medical conditions to speed verification and pre-authorization calls.
| Payment Type | Typical Coverage/Requirement | Action Steps to Verify |
|---|---|---|
| Commercial Insurance (examples listed) | Coverage varies; may require pre-authorization and medical necessity documentation | Call the insurer with treatment codes and dates; provide clinical details to admissions for verification |
| TRICARE | May require authorization and coordination with military benefits | Contact TRICARE and share the proposed treatment plan; coordinate with admissions for pre-authorization |
| Private Pay | Immediate start may be possible with upfront payment arrangements | Discuss rates and payment plans with admissions; prepare ID and financial documentation |
This table clarifies verification pathways and helps prospective patients take next steps with confidence.
Which Insurance Providers Does BetterChoice Accept for Detox?
Insurers noted as accepted include Magellan Health, TRICARE, Aetna, Anthem, Blue Cross Blue Shield, Beacon Health Options, Cigna, and EmblemHealth. Coverage levels and network participation still vary by plan and state. Facility acceptance means we can bill these insurers, but you must confirm that your specific plan, benefit level, and medical necessity requirements are met for detox services. Admissions typically ask for your insurance card and recent medical history to start benefit checks and determine prior authorization needs. Verifying benefits before arrival reduces delays and clarifies any patient financial responsibility.
This list helps readers identify likely insurer partners and leads into an admissions checklist.
How Can Patients Verify Coverage and Start Admissions?
To begin admissions, follow a simple verification checklist: gather insurance and medical information, call your insurer for benefit details, and provide documentation to the treatment provider so the admissions team can run a confidential benefits check and request pre-authorization if needed. Bring identification, a list of current medications, and any recent clinician notes to speed clinical screening and authorization. For local admissions, contact the center by phone or visit the facility to arrange assessment and logistics; record verification conversations and authorization numbers for your records. Doing these steps early reduces administrative delays and lets clinical staff focus on safe stabilization and transition planning.
Practical admissions checklist:
- Provide your insurance card and medical history for benefits verification.
- Request pre-authorization if required and obtain authorization numbers.
- Coordinate transportation and personal belongings for admission day.
These steps help ensure a smoother transition into medically supervised detox at the facility.
198 Ebb Tide Cir, Las Vegas, NV 89123 and phone (725) 299-4777 are listed contact points for logistical and admissions inquiries; families can use these channels to request confidential benefit checks and begin coordination with clinical staff.
Frequently Asked Questions
What should I expect during the intake process for opioid detox?
Expect a thorough clinical assessment during intake: a review of medical history, current medications, and any psychiatric conditions; vital signs checks; and possibly laboratory testing to establish a health baseline. This evaluation lets the clinical team tailor the detox plan to the individual’s needs for a safer, more effective start to treatment.
How can I support a loved one going through opioid detox?
Support looks like practical help and steady presence: gather medical records and medication lists, coordinate transportation for admission and discharge, and join family education sessions if invited. Emotional support reduces anxiety and encourages the person to engage with treatment — both of which matter during detox.
What role does medication-assisted treatment (MAT) play in detox?
MAT helps ease withdrawal symptoms and reduce cravings, making stabilization and the transition to recovery more manageable. Medications like buprenorphine are commonly used alongside counseling and behavioral therapies to address both physical dependence and underlying behavioral health needs.
What are the potential risks of unsupervised opioid withdrawal?
Unsupervised withdrawal can lead to severe dehydration, unstable vital signs, and a higher risk of relapse or overdose after tolerance falls. Without medical oversight, intense symptoms and co-occurring health issues can lead to complications that supervised detox is designed to prevent.
How does family involvement impact recovery outcomes?
Family involvement improves outcomes by providing emotional support, reinforcing treatment plans, and helping create a safer post-discharge environment. Education about addiction and communication strategies can reduce conflict and increase the chance of sustained engagement in follow-up care.
What should I know about the costs associated with opioid detox?
Detox costs vary based on provider, insurance coverage, and services required. Verify your benefits and any out-of-pocket costs before admission. Many centers, including BetterChoice, assist with insurance navigation and payment options to clarify financial responsibilities.
What aftercare options are available following detox?
After detox, options include inpatient rehabilitation, outpatient therapy, counseling, and peer support groups. Transition planning typically starts during detox so patients move seamlessly into the next level of care. Engaging in aftercare is essential for maintaining recovery and addressing underlying issues related to addiction.
Conclusion
Choosing a medically supervised opioid detox program in Summerlin gives people the safety, medical oversight, and clear next steps they need to begin recovery. With continuous monitoring, individualized care plans, and access to Medication-Assisted Treatment, patients can get through withdrawal more safely and move into ongoing support. Families play a vital role in this process through practical help and education. Take the next step—contact BetterChoice Treatment Center to learn how we can help you or a loved one begin recovery.
