
Dopamine & Addiction: Understanding the Brain’s Reward System — What It Means for Treatment
Dopamine is a key brain chemical that helps drive motivation, reinforcement, and expectations about reward. When dopamine signaling is disrupted, it plays a central role in how addiction starts and why it can be so persistent. This article breaks down the neuroscience behind the brain’s reward circuits, how substances and behaviors hijack those pathways, common clinical signs of dopamine imbalance, and evidence-based treatments that support recovery. You’ll find clear explanations of the brain regions and neurotransmitters that interact with dopamine, the behavioral and physical cues that suggest dysregulation, and practical treatment pathways that help stabilize brain chemistry and restore function. We also outline typical timelines for receptor recovery, list therapies that encourage neuroplasticity, and offer concrete guidance families can use to support a loved one seeking care. Sections include: what dopamine does, how addiction alters the mesolimbic pathway, observable signs of imbalance, how clinical care addresses these changes (including medical detox and inpatient care), realistic healing timelines, and steps families can take to facilitate treatment and recovery.
What is Dopamine and How Does it Regulate the Brain’s Reward System?
Dopamine is a chemical messenger made by specific neurons that signals reward prediction, motivation, and how important a stimulus is. It helps the brain learn which actions lead to good outcomes and reinforces those behaviors. In practice, dopamine release along the mesolimbic pathway — mainly from the ventral tegmental area (VTA) to the nucleus accumbens (NAc) — flags unexpected rewards or cues that predict reward. Those signals change synaptic strength and influence which actions get repeated. When dopamine signaling is balanced, it supports goal-directed behavior and sound decision-making; when it is too high or too low, motivation and enjoyment can shift dramatically. That regulatory role explains why repeated drug-driven dopamine spikes cause lasting behavioral change and why treatment focuses on both normalizing brain chemistry and relearning healthy responses.
Dopamine supports everyday behavior through several core roles:
- Motivation and goal-directed behavior: dopamine helps energize pursuit of important outcomes.
- Reinforcement learning: quick dopamine bursts mark prediction errors and update future choices.
- Motor and cognitive modulation: dopamine influences movement, attention, and working memory.
These roles explain ordinary reward-driven activities — eating, social connection, achievement — and help us see how drugs create maladaptive reinforcement that often requires clinical care.
In treatment settings, clinicians address both the chemical imbalance and the learned behaviors that sustain compulsive use.
How Does Dopamine Function as the Brain’s Pleasure Chemical?
Calling dopamine the brain’s “pleasure chemical” is an oversimplification. Dopamine is best understood as a learning and motivation signal: it tells the brain what to pursue and when to expect a reward, more than it directly creates pleasure. Rapid, phasic dopamine bursts occur with unexpected rewards or cues that predict reward, while tonic dopamine sets a baseline tone that shapes overall responsiveness and drive. Think of it like a reward prediction error: a better-than-expected outcome gives a burst that strengthens the behavior that led to it; a worse-than-expected outcome weakens that link. This learning-centered view explains why substances that cause large phasic spikes form strong habits and why people in recovery can experience low motivation or “anhedonia” while the system recalibrates.
The distinction between phasic and tonic signaling matters for treatment: stabilizing baseline dopamine and reducing cue-driven spikes helps lower compulsive responding. That’s why effective programs combine medical management with behavioral therapies to rebuild healthy reward associations.
Which Neurotransmitters Work Alongside Dopamine in Addiction?
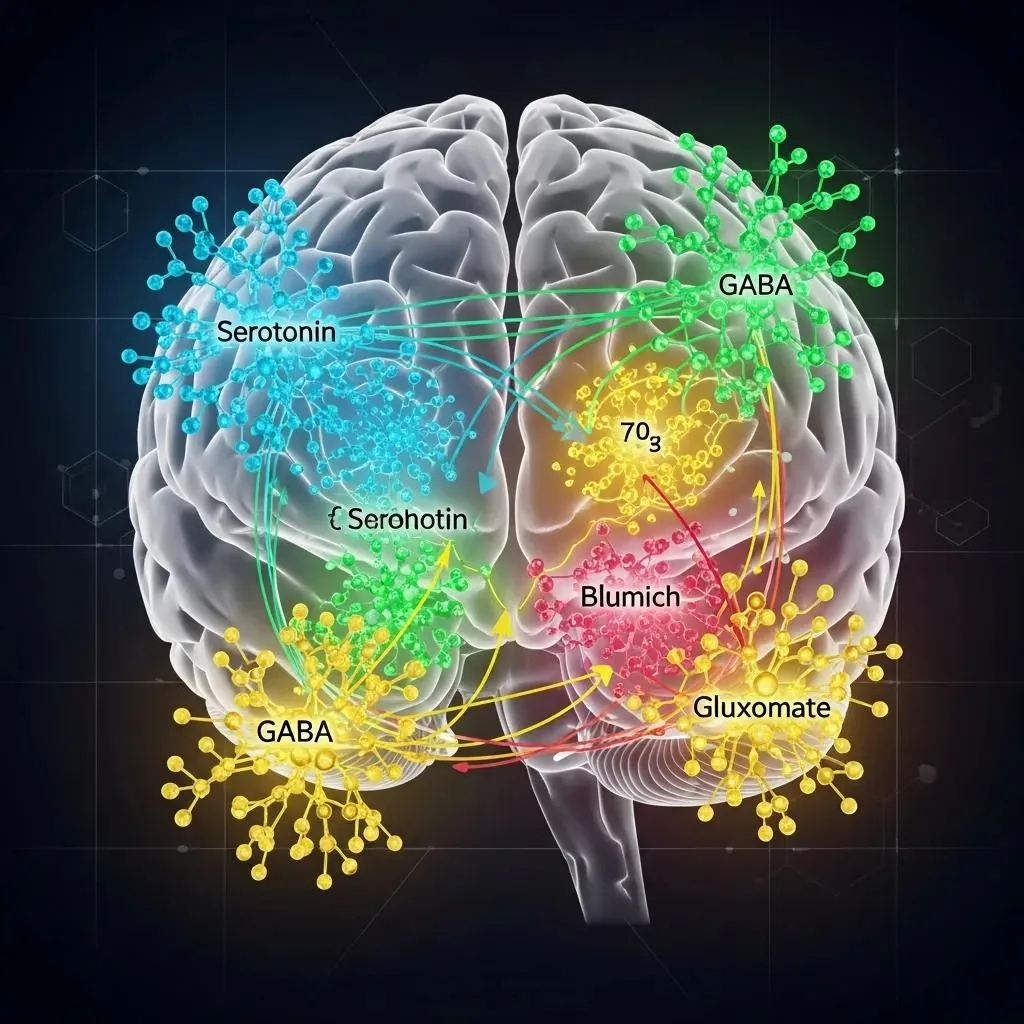
Dopamine does not act alone. Several other neurotransmitter systems shape inhibition, excitation, and mood — and together they influence how addiction develops and how withdrawal looks. Key partners include serotonin (mood and impulse control), GABA (inhibitory tone that limits overactivity), glutamate (excitatory plasticity that drives learning), and norepinephrine (arousal and stress responses). Each system changes how dopamine-driven learning happens: for example, glutamate helps lock in drug-cue memories, and reduced GABAergic tone can increase impulsivity and compulsive responding.
- Serotonin: affects mood and impulse regulation and can alter relapse risk when disrupted.
- GABA: provides inhibitory control over reward circuits; imbalance can raise compulsivity.
- Glutamate: enables synaptic changes that cement drug-associated memories and cravings.
Seeing addiction as a polychemical problem explains why evidence-based care often targets multiple systems — using medication, behavioral therapy, and supportive interventions — to reduce craving and restore long-term function. It also clarifies why some treatments focus on glutamatergic or GABAergic pathways in addition to stabilizing dopamine.
How Does Addiction Hijack the Brain’s Reward Pathway?
Addiction hijacks reward circuitry by producing repeated, supra-physiological dopamine surges that train the brain to prioritize drug-related cues and behaviors over natural rewards. Powerful phasic dopamine releases caused by drugs or addictive behaviors create prediction errors that bias learning toward substance-seeking. Over time the brain adapts — receptors downregulate, synapses rewire — producing tolerance, stronger cue reactivity, and compulsive use despite harmful consequences. Behavior shifts from voluntary use to habit-driven or compulsive patterns, decision-making weakens, and relapse risk rises.
Below is a clinician-style comparison showing how common substances differ in their effects on dopamine release, tolerance timelines, and withdrawal risk to help guide treatment planning and expectations.
Different substances alter dopamine signaling and clinical risk in distinct ways.
| Substance Class | Typical Dopamine Effect | Clinical Timeline / Withdrawal Risk |
|---|---|---|
| Stimulants (e.g., methamphetamine, cocaine) | Rapid, large phasic dopamine surges in NAc | Rapid tolerance; intense cravings; high relapse risk; withdrawal includes fatigue and depression |
| Opioids (e.g., heroin, fentanyl) | Indirect dopamine increase via opioid receptors | Tolerance grows over weeks; high physical withdrawal risk requiring medical management |
| Alcohol | Modulates GABA/glutamate and increases dopamine indirectly | Progressive tolerance; withdrawal can be medically dangerous (seizure risk, delirium tremens) |
| Cannabis | Modest dopamine modulation, complex CB1-mediated effects | Variable tolerance; withdrawal often milder but includes irritability and sleep disturbance |
What Roles Do the VTA and Nucleus Accumbens Play in Addiction?
The Ventral Tegmental Area (VTA) contains dopamine-producing neurons that project to the Nucleus Accumbens (NAc), forming the core reward pathway tied to reinforcement and motivation. The VTA emits phasic dopamine bursts for rewards or predictive cues, and the NAc integrates those signals with glutamatergic input from cortical and limbic regions to guide approach behavior. Repeated drug exposure strengthens VTA→NAc signaling and the synaptic connections that link cues to substance-seeking, tilting behavior toward immediate reward instead of long-term goals.
Knowing these roles helps explain why treatment focuses on reducing cue-driven activation (with behavioral strategies) and stabilizing VTA/NAc function (with medical and supportive care). Lowering cue salience and rebuilding other sources of reward are core parts of restoring balanced motivation.
How Does Addiction Affect Decision-Making in the Prefrontal Cortex?
The Prefrontal Cortex (PFC) provides executive control over impulses, planning, and evaluating consequences. Chronic substance use weakens PFC activity and its connectivity with reward circuits, impairing inhibition, future-oriented thinking, and flexible decision-making. Clinically, this looks like impulsivity, poor planning, and a tendency to choose immediate relief despite serious long-term costs.
Rehabilitative work focuses on strengthening PFC skills — cognitive control, delay of gratification, problem solving — through cognitive therapies and structured routines that promote executive recovery. Restoring PFC function is essential so reduced biological craving translates into sustained behavior change.
What Are the Signs and Symptoms of Dopamine Imbalance in Addiction?
Dopamine imbalance in addiction produces a recognizable cluster of behavioral, emotional, and physical signs clinicians and families can watch for. Behaviorally, someone may show intense craving, compulsive seeking, and reduced interest in previously enjoyable activities (anhedonia). Emotionally, mood swings, irritability, anxiety, and depressive symptoms are common as reward sensitivity shifts. Physically, look for sleep disruption, appetite changes, fatigue, and withdrawal-related symptoms — some of which require medical attention.
The lists below separate the most common behavioral/emotional and physical signs for quick clinical recognition.
Top behavioral and emotional signs linked to dopamine dysregulation include:
- Craving and compulsive use: Persistent, intrusive desire to obtain and use the substance despite harm.
- Anhedonia: Less pleasure from normally rewarding activities because reward sensitivity is lowered.
- Mood instability: Increased irritability, anxiety, or depressive symptoms as baseline dopamine tone shifts.
These behavioral indicators often trigger clinical assessment and triage because they reflect both neurobiological change and functional impairment. Spotting them early supports timely referral to stabilization and treatment services.
Which Behavioral and Emotional Symptoms Indicate Dopamine Dysregulation?
Behavioral and emotional symptoms align with underlying dopamine changes: intense cue-driven pursuit reflects phasic oversignaling, while anhedonia corresponds to receptor downregulation and lower tonic tone. People may cycle between hyper-focused drug-seeking and low-motivation, depressed states when not using. Clinically, these patterns signal relapse risk and point to the need for combined behavioral relearning and biological stabilization.
One common scenario: a person who once enjoyed hobbies stops attending them and spends increasing time seeking drugs. That shift reflects both altered reinforcement learning and weakened alternative reward pathways, and it highlights the need for therapeutic work to rebuild non-drug rewards.
What Physical Manifestations Result from Dopamine Addiction?
Physical signs tied to dopamine-related addiction include sleep problems, appetite and weight changes, chronic fatigue, and substance-specific withdrawal symptoms. Some withdrawals (for example, alcohol or opioids) carry serious medical risks — seizures or severe autonomic instability — and require supervised detox. Monitoring physical cues like persistent insomnia, marked weight loss, or autonomic symptoms helps families and clinicians decide when medical care is needed.
Early medical stabilization addresses acute physiological risks while psychosocial supports begin behavioral recovery. Knowing the likely physical course for a given substance informs safety planning and the level of supervision needed during early abstinence.
How Does BetterChoice Treatment Center Address Dopamine Addiction?

BetterChoice Treatment Center combines medical care and evidence-based therapies to treat both the neurobiological and behavioral sides of dopamine-driven addiction. Intake starts with a medical assessment to confirm physiological stability, screen for co-occurring mental health needs, and create an individualized plan that determines whether medical detox, inpatient care, or another path is best. Our clinical approach emphasizes evidence-based practices, personalized plans, integrated treatment for co-occurring conditions, and a multidisciplinary team of physicians, therapists, and nurses who provide around-the-clock support. BetterChoice maintains accreditations that reflect our clinical standards and support safe, medically supervised transitions through early recovery.
The table below compares medical detox and inpatient rehab from a clinician’s perspective so families understand what each service addresses in the brain and what to expect for monitoring and timelines.
Practical comparison of detox and inpatient rehab helps set expectations during early treatment.
| Service | What it affects in the brain/behavior | Typical timeline / Safety notes |
|---|---|---|
| Medical detox | Stabilizes physiology, manages acute withdrawal, begins normalization of neurotransmitter balance | Short-term (days to 1–2 weeks); requires medical monitoring for high-risk withdrawals |
| Inpatient rehab | Supports neuroplastic recovery, teaches coping skills, and reduces cue exposure while rebuilding routines | Usually weeks to months; offers structured therapy and 24/7 supervision to reduce relapse risk |
| Integrated care (detox→inpatient) | Combines physiological stabilization with behavioral relearning to maximize receptor recovery potential | Sequential approach: detox first, then inpatient or outpatient treatment as clinically indicated |
How Does Medical Detox Help Reset Brain Chemistry?
Medical detox provides controlled management of withdrawal and physiological stabilization to lower immediate medical risk and begin early neurotransmitter recovery. Under medical supervision, clinicians monitor vitals, treat severe symptoms, and use evidence-based medications when appropriate to reduce autonomic instability and intense discomfort. That safe, monitored window gives the brain a clearer baseline and lets psychosocial therapies be more effective. Families should expect continuous monitoring, a clear focus on safety, and coordinated follow-up planning to transition into longer-term care.
Detox is the first step in a staged approach: once physiology is stable, treatment shifts toward relearning, skill-building, and relapse prevention in a therapeutic setting.
What Behavioral and Holistic Therapies Support Brain Recovery?
Behavioral therapies rebuild adaptive reward learning, strengthen executive control, and encourage neuroplastic changes that support lasting recovery. Evidence-based psychotherapies commonly used include cognitive-behavioral therapy (CBT) for skills training, motivational interviewing to increase engagement, and elements of dialectical behavior therapy (DBT) for emotion regulation. These approaches address decision-making, craving management, and relapse prevention. Complementary supports — mindfulness, regular exercise, sleep hygiene, and nutrition — augment biological recovery by improving mood regulation, lowering stress-driven relapse triggers, and supporting synaptic health.
- Typical program structure: a mix of individual and group sessions multiple times per week, with family involvement when appropriate.
- Holistic supports aim to restore healthy reward pathways by encouraging natural reinforcers like social connection and physical activity.
Together, behavioral and holistic therapies speed the formation of new, non-drug reward associations and strengthen prefrontal control over impulsive drives.
Can Dopamine Receptors Heal After Addiction and How?
Yes. Dopamine receptors and related circuits can recover through neuroplastic processes, though timelines differ by substance, length of use, and individual factors. Neuroplasticity allows synapses to remodel, receptors to upregulate, and prefrontal control networks to reconnect when drug exposure stops and adaptive behaviors are learned. Research shows measurable improvements in receptor sensitivity and functional connectivity within months, with continued progress over many months to a year or longer — especially when therapy and healthy lifestyle changes are added. The evidence supports a model where biological recovery and behavioral reconditioning work together to restore balanced reward processing.
The table below links recovery activities to neurobiological mechanisms and realistic effects to help prioritize aftercare planning.
Mapping therapeutic activities to neuroplastic effects clarifies how recovery interventions support receptor and functional healing.
| Recovery Activity | Neurobiological Mechanism | Expected Effect / Timeline |
|---|---|---|
| Structured psychotherapy (CBT) | Promotes synaptic remodeling via repeated learning and inhibitory control strengthening | Improved cognitive control and reduced cue-reactivity over weeks to months |
| Regular aerobic exercise | Increases neurotrophic factors and dopamine receptor sensitivity | Mood and motivation improvements within weeks; sustained benefits over months |
| Sleep optimization | Restores homeostatic neurotransmitter balance and supports synaptic consolidation | Faster mood stabilization; sleep improvements seen in weeks |
| Nutritional support | Provides precursors and cofactors for neurotransmitter synthesis | Incremental improvements in energy and mood within weeks |
| Medication-assisted stabilization (as clinically appropriate) | Reduces withdrawal-driven dopamine dysregulation and craving | Immediate symptom reduction; supports longer-term plasticity when combined with therapy |
What Is Neuroplasticity and Its Role in Dopamine Receptor Recovery?
Neuroplasticity is the brain’s ability to reorganize connections in response to experience, learning, and environmental change. It’s the engine behind receptor and circuit recovery after stopping substances. Through repeated practice of new behaviors, therapy-based cognitive strategies, and supportive lifestyle changes, synaptic strengths shift to favor non-drug rewards and strengthen top-down control. Clinically, that looks like reduced craving, better decision-making, and renewed ability to enjoy everyday activities. Prioritizing neuroplastic interventions — consistent therapy, exercise, and good sleep — speeds functional recovery and helps lock in healthier neural pathways.
In short: recovery is possible, but it takes sustained, targeted practice to replace drug-associated learning with adaptive alternatives.
How Long Does It Take for Dopamine Levels to Normalize?
TImelines vary. Acute withdrawal and early stabilization usually occur over days to weeks. Partial receptor sensitivity and mood improvements often appear over several months, and more complete functional recovery can continue across six months to a year or longer. Factors that affect pace include substance type (stimulants and opioids often show longer recovery curves), duration and intensity of use, co-occurring mental health conditions, age, and whether the person has structured aftercare. Active participation in evidence-based therapy, regular exercise, healthy sleep, and good nutrition all help accelerate normalization and functional gains.
Realistic timelines set expectations: detox and early therapy bring quick relief and reduced medical risk, while cognitive and hedonic restoration require sustained effort and support over months.
How Can Families Support Loved Ones Understanding Dopamine and Addiction?
Families play a vital role by turning neurobiology into practical, compassionate action: learning how the reward system drives behavior, setting supportive boundaries, and helping with logistics to get care. Understanding that addiction rewires learning — so drug cues trigger strong cravings — reduces blame and reframes addiction as a treatable brain process rather than a moral failing. Practical family steps include gathering medical information for intake, arranging safe transportation, checking insurance details, and preparing to support aftercare while maintaining healthy boundaries.
The checklist below offers actionable steps families can take when arranging treatment and supporting early recovery.
Checklist families can use to facilitate care engagement and early recovery support:
- Verify immediate safety and medical stability before transport.
- Prepare information on substance use history and any co-occurring mental health conditions for intake.
- Call the treatment provider to discuss intake process, insurance considerations, and program options.
- Arrange transportation, a small set of belongings, and clear communication preferences for the initial admission.
This practical checklist reduces the logistical barriers that often delay care. Calm, informed family involvement increases the chance of a timely and successful treatment engagement.
What Should Families Know About the Brain’s Reward System?
Families should know that the brain’s reward system learns associations: addiction skews those associations so drug-related cues trigger disproportionate craving and action. Explaining that dopamine supports learning and motivation — rather than only producing pleasure — helps families understand why a loved one may persist in harmful behavior and why change requires structured support instead of simple willpower. Avoid blaming language; instead, focus on how treatment rebuilds alternative reward pathways and executive control through proven interventions.
When families frame conversations around brain science and recovery strategies, they become better advocates who offer practical help without unintentionally enabling harmful patterns.
How Can Families Facilitate Treatment and Recovery Support?
Families can make treatment easier by preparing for intake, asking specific questions about safety and aftercare, and planning supportive but firm boundaries that prioritize health. Useful intake questions include which medical assessments will be done, how co-occurring mental health needs are handled, and what follow-up supports look like. Expect programs that offer integrated care, a multidisciplinary team, and 24/7 supervision during high-risk phases; clarify visiting policies and privacy expectations ahead of time.
If you need help initiating care or navigating intake, call the provider’s intake line to discuss next steps and insurance guidance: (725) 299-4777. Practical coordination and steady emotional support speed access to safe, evidence-based treatment while protecting family wellbeing.
- Prepare documentation: List medications, history of use, and relevant medical information.
- Coordinate logistics: Arrange transport and a safe plan for admission day.
- Set expectations: Understand program structure, visiting rules, and aftercare requirements.
These steps reduce confusion during a stressful time and support a smoother transition into care and a more sustainable recovery process.
Frequently Asked Questions
What are the long-term effects of dopamine dysregulation on mental health?
Long-term dopamine dysregulation can contribute to persistent mental health challenges, including chronic anxiety, depression, and mood instability. Because dopamine helps regulate motivation and reward, its imbalance can cause ongoing anhedonia and difficulties with decision-making and impulse control. These issues can complicate recovery, which is why comprehensive treatment plans often include targeted mental health care alongside addiction treatment.
How can lifestyle changes support dopamine recovery?
Healthy lifestyle changes play an important role in dopamine recovery. Regular aerobic exercise boosts neurotrophic factors and can increase dopamine receptor sensitivity. A balanced diet supplies the nutrients needed for neurotransmitter synthesis. Consistent sleep and stress-reduction practices such as mindfulness also support mood and motivation. Together, these habits reinforce healthier reward pathways and support long-term recovery.
What role does therapy play in dopamine addiction recovery?
Therapy is a foundation of recovery. Evidence-based approaches like cognitive-behavioral therapy (CBT) help people identify and change thought patterns and behaviors tied to substance use. Therapy teaches coping strategies for cravings, improves emotional regulation, and helps rebuild motivation for non-drug rewards. When combined with medical care and lifestyle supports, therapy strengthens the neural and behavioral changes needed for sustained recovery.
Can dopamine levels return to normal after prolonged substance use?
Yes — but timelines vary. Neuroplasticity allows the brain to recover, and many people show measurable improvements in receptor sensitivity and function within months of abstinence. Factors such as substance type, length of use, co-occurring conditions, and age affect recovery speed. Engaging in structured therapy, healthy lifestyle changes, and ongoing support can accelerate normalization and improve emotional and cognitive functioning over time.
What are the signs that someone is experiencing dopamine withdrawal?
Dopamine withdrawal can show up emotionally and physically. Common signs include intense cravings, fatigue, irritability, mood swings, and anhedonia. Physical symptoms often include sleep disruption, appetite changes, and general malaise. Recognizing these signs early is important because they indicate the need for medical and therapeutic support to manage withdrawal safely and promote recovery.
How can families help loved ones during recovery from dopamine addiction?
Families can support recovery by offering steady emotional support, practical assistance, and informed advocacy. Learning about addiction and its effects reduces stigma and promotes compassion. Families should encourage open communication, set healthy boundaries, and help with logistics like transportation and aftercare planning. Active, informed family involvement can significantly improve recovery outcomes.
Conclusion
Understanding how dopamine and the brain’s reward system interact with addiction helps guide effective treatment and recovery. By recognizing signs of dopamine imbalance and the roles of other neurotransmitters, families and individuals can make informed decisions about care. Evidence-based therapies combined with lifestyle changes improve outcomes and support long-term recovery. For more information on how to support yourself or a loved one, explore our resources or contact our intake team.
