
Codependency & Addiction Treatment: Break Unhealthy Patterns and Build Lasting Recovery
Codependency describes patterns where your sense of worth and emotional stability rely heavily on another person’s needs or approval. It often appears alongside substance use disorders and can keep families stuck in cycles that block recovery. This guide walks you through how codependency and addiction interact, how unhelpful family roles form, and practical, evidence-based steps to change those patterns for good. You’ll learn how to spot common signs of codependency, recognize enabling behaviors that maintain substance use, and compare treatment choices—medical detox, inpatient care, dual-diagnosis programs, and family therapy. We also outline therapeutic approaches like CBT, DBT, trauma-informed care, and peer support, and give clear, actionable strategies for setting boundaries, practicing self-care, and finding local help. Throughout, the guidance reflects current clinical practice and research so individuals and families can evaluate options and plan next steps toward healthier relationships and recovery.
What is codependency, and how does it affect addiction?
Codependency is a pattern of excessive emotional reliance on another person, often showing up as caretaking that sacrifices your own needs to help someone who’s using substances. That caretaking can unintentionally reinforce the substance use—short-term relief or protection removes consequences and lowers the person’s motivation to change. Addressing codependency directly improves treatment outcomes for the person with substance use disorder and reduces relapse risk across the family system.
The sections that follow define codependency more precisely and list practical signs to help you see whether these patterns are present in your relationships.
Defining codependency: relationship addiction and enabling behaviors
Codependency—sometimes called relationship addiction—describes habitual behaviors where one person consistently puts another’s needs above their own health and autonomy. Clinicians often view it as a learned coping style (people-pleasing, excessive caretaking, attempts to control outcomes) that grows out of childhood instability or trauma. Those behaviors are reinforcing because they ease immediate distress for both people: the caretaker feels needed and the person using substances avoids consequences. Framing codependency as a behavioral pattern—not a moral failing—lets treatment focus on practical skill-building: restoring boundaries, improving self-regulation, and reclaiming personal agency.
Recognizing signs of codependency in relationships
Spotting codependent patterns means honestly tracking repeated behaviors that hurt your well-being and independence. Common signs include chronic people-pleasing, trouble saying no, taking responsibility for others’ choices, low self-worth tied to caretaking, and avoiding conflict to keep peace. Ask yourself: Do you feel guilty when you put yourself first? Do you step in to rescue others even when it harms you financially or emotionally? Naming these patterns is the first step toward targeted therapy that rebuilds autonomy and reduces enabling behaviors that sustain addiction.
How does codependency fuel addiction and dysfunctional family patterns?
Codependency and addiction reinforce one another: caretaking shields the person using substances from natural consequences, and the ongoing use deepens family role adaptations. Over time roles like “rescuer,” “enabler,” or “identified patient” become fixed, which makes recovery harder because family members are unintentionally maintaining the problem. Breaking the cycle requires stopping enabling behaviors, improving communication, and setting consistent consequences that encourage treatment engagement. The next sections unpack the step-by-step dynamics of this cycle and identify common enabling behaviors and their effects on recovery.
Understanding the cycle of codependency and addiction
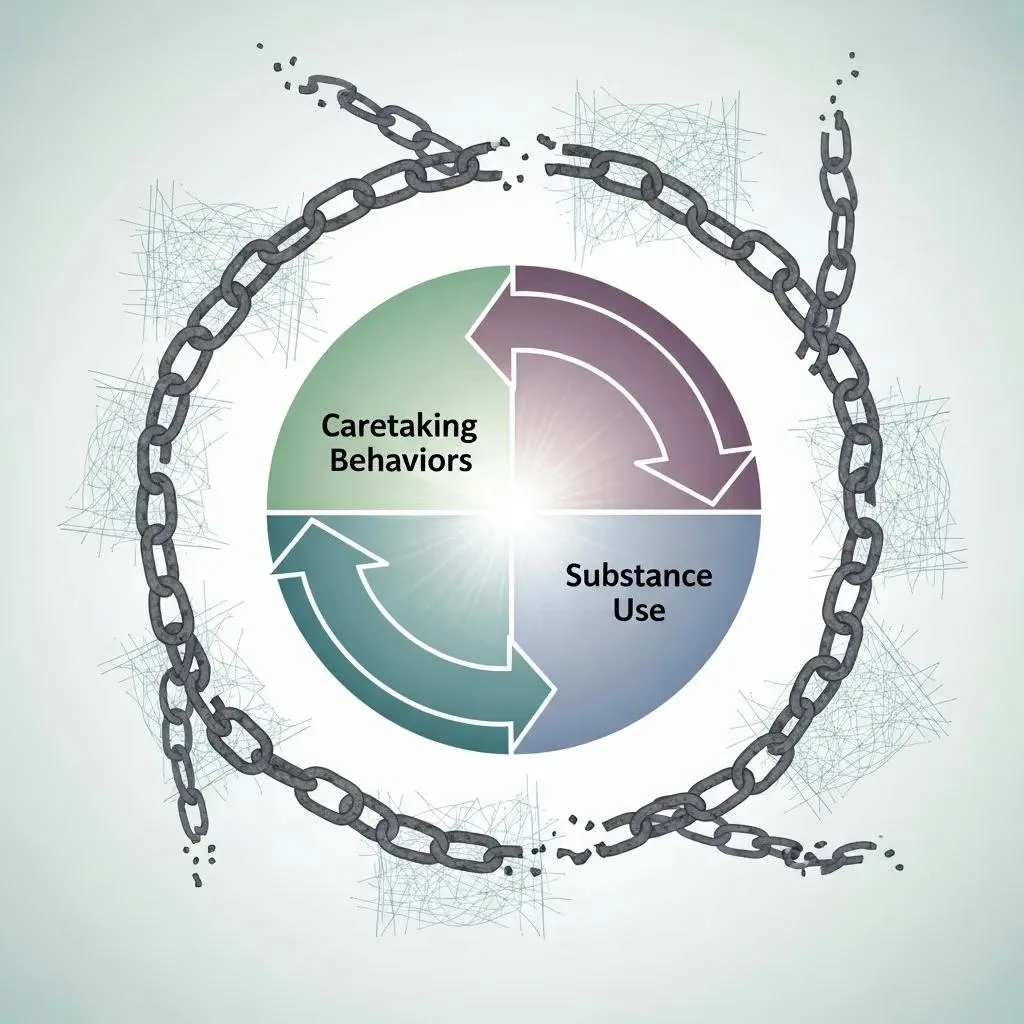
The cycle often starts with family stress or early trauma, followed by one member using substances to cope and another responding by minimizing consequences to keep short-term stability. That pattern—stress → substance use → caretaking → avoidance of accountability—repeats and escalates, embedding dysfunction into everyday life. Families adopt rigid roles that resist change, and secrecy, denial, or mixed expectations can undermine treatment. Recognizing each step helps clinicians and families choose interventions that target the specific link—trauma-informed therapy, boundary-setting, and relapse prevention planning.
Identifying enabling behaviors and their impact on recovery
Enabling behaviors protect the person with addiction from natural consequences and reduce their incentive to seek help. Common examples include making excuses for missed work, covering financial shortfalls, hiding substance use, and taking on responsibilities the person should handle. Each enabling action prolongs dependence, raises relapse risk, and drains emotional and material resources. Stopping these behaviors is painful but necessary; when families replace enabling with clear limits, treatment engagement and long-term recovery outcomes improve.
What treatment options are effective for codependency and addiction?
Effective, evidence-based care for co-occurring codependency and substance use spans a continuum: medical detox for safe withdrawal, inpatient rehab for intensive stabilization, outpatient programs for skills and maintenance, family therapy to repair relational patterns, and peer support for ongoing recovery. Which path fits depends on the severity of substance use, co-occurring mental health conditions, safety concerns, and family involvement. The table below summarizes typical attributes across common levels of care to help you compare options.
Different levels of care balance safety, therapy intensity, and supervision.
| Level of Care | Typical Length | Level of Supervision | Best For |
|---|---|---|---|
| Medical Detox | 3–7 days | Continuous medical monitoring for withdrawal | Individuals with physiological dependence needing safe withdrawal |
| Inpatient Rehab | 2–6 weeks (typical) | 24/7 clinical and nursing support | People needing structured environment and intensive therapy |
| Outpatient Program | Weeks to months | Scheduled therapy and medical visits | Stable individuals with support and lower medical risk |
| Counseling / Family Therapy | Ongoing | Session-based clinical care | Families and individuals addressing relational patterns and skills |
This comparison highlights how each approach trades off intensity, oversight, and therapeutic focus so you can choose a path that fits clinical needs and life circumstances.
Medical detox and inpatient rehab programs at BetterChoice
Medical detox and inpatient rehab offer structured, medically supervised care that prioritizes safety, withdrawal management, and early stabilization for people with moderate to severe dependence. During detox, clinicians monitor vital signs, manage withdrawal symptoms, and may use medications to reduce risk. Inpatient rehab adds daily individual and group therapy, psychiatric evaluation when needed, and round‑the‑clock staff to support stabilization and the first stages of recovery.
BetterChoice Treatment Center in Las Vegas, Nevada provides integrated medical detox and inpatient services with privacy protections, 24/7 supervision, and coordinated transition planning to the next level of care.
| Program Element | Typical Process | What to Expect |
|---|---|---|
| Intake Assessment | Clinical and medical evaluation on admission | Personalized risk assessment and initial treatment plan |
| Medical Management | Ongoing monitoring during withdrawal | Medication-assisted management and nursing oversight |
| Therapy Schedule | Daily group and individual sessions | Psychoeducation, coping skills, and relapse prevention |
This outline clarifies intake and clinical steps, helping families and individuals know what to expect while emphasizing safety, individual planning, and respect for privacy.
Dual diagnosis treatment: addressing co-occurring mental health disorders
Dual diagnosis care combines psychiatric treatment with addiction services so mental health issues and substance use are treated together. Untreated conditions like anxiety, depression, or trauma-related disorders increase relapse risk, so integrated plans include psychiatric assessment, medication when appropriate, therapy approaches that address both conditions, and coordinated case management. Treating the whole person—mental health, trauma, and relational patterns—improves engagement in recovery and supports lasting functioning by reducing triggers and strengthening new relational skills.
How does family therapy support recovery from codependency and addiction?

Family therapy targets the relational patterns that keep codependency and addiction going by improving communication, clarifying roles, and teaching behavioral tools that reduce enabling. Models like structural family therapy, behavioral family therapy, and multi-family groups use different techniques but share goals: set healthy boundaries, rebuild trust, and encourage recovery-supportive behaviors. Family work is linked to lower relapse rates, better treatment adherence, and stronger family functioning. The sections below explain how sessions are structured and what benefits families commonly see.
Healing relational patterns through family therapy
Family therapy focuses on real interactions, teaching members to swap enabling responses for consistent, healthier choices through role-play, communication training, and problem-solving drills. Therapists help families create clear relapse-prevention plans and rehearse difficult conversations in a safe setting. Sessions aim to define expectations, assign responsibilities, and practice boundary enforcement so new habits carry over at home. Over time these practices reduce secrecy, increase accountability, and rebuild trust—key supports for the person in treatment and for reducing codependent dynamics.
Benefits of family support in breaking unhealthy patterns
When families align the home environment with treatment goals, recovery accelerates and triggers that spark relapse decrease. Many families notice clearer roles, fewer crisis rescues, better communication, and more engagement in aftercare within weeks to months of consistent therapy. These changes translate into measurable outcomes: improved medication adherence, higher attendance in outpatient programs, and fewer emergency interventions. Families can choose in-person sessions, multi-family groups, and privacy safeguards to protect sensitive information during treatment.
Which therapeutic modalities help in codependency recovery?
Several evidence-based therapies address the thinking, emotions, and behaviors that maintain codependency and addiction. Cognitive Behavioral Therapy (CBT) helps reframe distorted thoughts that drive people-pleasing; Dialectical Behavior Therapy (DBT) teaches emotion regulation and distress tolerance; trauma-informed care recognizes and stabilizes the impact of past trauma. Peer support and community resources add ongoing social reinforcement for new behaviors. The sections below outline individual therapy approaches and the role peer groups play in maintaining gains.
Individual therapy approaches: CBT, DBT, and trauma-informed care
Individual therapy gives focused work on the beliefs and skills that sustain codependency. CBT helps identify and change cognitive distortions—thoughts like “I’m only valuable if I fix others”—and uses behavioral experiments to practice alternatives. DBT adds training in emotion regulation, interpersonal effectiveness, and distress tolerance, which is helpful when caretaking coexists with strong emotional reactivity. Trauma-informed care ensures clinicians recognize past adversity, build stabilization skills before deep processing, and prioritize safety and empowerment. Together, these approaches increase boundary-setting and self-efficacy.
Group therapy and support groups: CoDA, Al-Anon, and Nar-Anon
Group therapy and peer support reduce isolation and offer a place to practice boundaries among people with similar experiences. Clinically led groups focus on skill-building—communication, relapse prevention, and relationship homework—while community groups like CoDA and Al-Anon provide ongoing mutual support and accountability. Meetings model healthier interactions and reinforce new skills learned in individual therapy. When paired with clinical care, peer groups extend support beyond the clinic and help sustain long-term recovery through shared experience.
What practical steps can individuals take to break codependent patterns?
Changing codependent patterns takes concrete actions: notice the habits that harm you, set and keep boundaries, start individual therapy, and build self-care routines that restore independence. Also consider joining peer support, taking part in family therapy, and coordinating care with providers who treat both addiction and mental health. The numbered checklist below is a starter plan you can begin this week, followed by guidance on boundary-setting and what to expect during professional intake.
- Recognize and name patterns: Keep a brief log of moments you prioritize others at your own expense and write specific examples.
- Set clear boundaries: Choose one concrete boundary to try this week and communicate it calmly and consistently.
- Seek individual therapy: Work with a clinician trained in CBT, DBT, or trauma‑informed care to build practical coping skills.
- Engage family support: Invite family members to join structured family therapy or educational sessions.
- Join peer groups: Attend CoDA, Al‑Anon, or similar meetings for ongoing mutual support.
These steps create an actionable roadmap. The next sections explain how to set boundaries and what professional intake typically looks like when you pursue formal treatment.
How to set healthy boundaries in recovery
Healthy boundaries start with naming the behaviors you will no longer accept, then communicating that limit in short, unemotional statements. Try scripts like, “I can’t give you money for substances; I will help you find treatment resources instead,” and be ready to follow through with consistent consequences if the boundary is tested. Expect resistance at first—changing relationship patterns shifts the balance of power—and plan gradual enforcement with support from a therapist or a support group. Consistent boundaries protect your recovery and help the other person take responsibility for their choices, which supports long-term relapse prevention.
Prioritizing self-care and personal growth for lasting change
Long-term change requires daily and weekly habits that rebuild identity, resilience, and life beyond caregiving. Create a self-care checklist—sleep routines, regular movement, mindfulness or meditation, therapy homework, and social activities that feed personal interests. Set measurable goals, such as a weekly class or volunteer commitment, to expand your sense of purpose outside caretaking roles. Track progress with a journal or therapist check-ins to keep momentum and reduce the chance of slipping back into old patterns.
If you’re ready to pursue professional help, a practical next step is contacting an accredited local program. BetterChoice Treatment Center helps people in Nevada find options quickly and provides clear guidance on available services; callers can reach our intake line at (725) 299-4777 to ask about program availability, privacy protections, and admission steps. Expect an initial phone assessment, scheduling of clinical and medical evaluations on arrival, and a personalized treatment plan developed with the care team to address both substance use and relational dynamics.
This resource combines current clinical approaches with practical actions to help individuals and families identify codependent patterns, see how those patterns fuel addiction, and choose appropriate levels of care. Below is a concise table summarizing common intake steps and required documentation to reduce friction when contacting a program for assessment and admission.
Clear intake steps make it easier to access care and set expectations for the first days of treatment.
| Step | Typical Timeline | Purpose |
|---|---|---|
| Initial Phone Screening | Same day to 48 hours | Assess immediate risk and match level of care |
| Clinical and Medical Assessment | Within 24–72 hours of admission | Create individualized treatment plan and safety plan |
| Admission Documentation | At intake | Confirm consent, medical history, and privacy preferences |
Knowing these steps helps families prepare practically and emotionally, reducing barriers to timely, confidential care.
Frequently asked questions
What are the long-term effects of codependency on mental health?
Left unaddressed, codependency can contribute to anxiety, depression, chronic low self-esteem, and identity confusion. People often tie their self-worth to meeting others’ needs, which can fuel ongoing emotional strain and burnout. Therapy and peer support can help rebuild a healthier sense of self and teach sustainable skills for setting limits and meeting personal needs.
How can I support a loved one in recovery from codependency and addiction?
Support looks like steady, nonjudgmental presence combined with clear boundaries. Listen without rescuing, offer resources, and encourage professional help. Educate yourself about both addiction and codependency so you know how to respond, and consider family therapy or support groups to learn effective ways to help while protecting your own well‑being.
What role does self-care play in overcoming codependency?
Self-care is essential: it restores a sense of autonomy and builds resilience against returning to caretaking habits. Regular practices—exercise, sleep, mindfulness, hobbies, and therapy homework—help you reconnect with your needs and reduce the impulse to over-function for others. Over time, consistent self-care supports healthier relationships and steadier recovery.
Are there specific support groups for codependency?
Yes. Co‑Dependents Anonymous (CoDA) focuses specifically on codependency recovery. Al‑Anon and Nar‑Anon support friends and family of people with substance use disorders, helping members address how a loved one’s use affects their lives. These groups offer peer connection, shared experience, and practical tools that complement clinical care.
How can I identify if I am in a codependent relationship?
Look for repeated patterns: feeling guilty when you assert yourself, regularly rescuing or enabling someone else, or basing your self-worth on being needed. If you avoid conflict at the expense of your own needs or feel responsible for another’s happiness, those are strong indicators of codependency. Reflecting on these signs with a therapist or trusted support can clarify next steps.
What are the benefits of dual diagnosis treatment for codependency and addiction?
Dual diagnosis programs treat mental health disorders and substance use together, which is critical because untreated psychiatric symptoms often drive relapse. Integrated care includes psychiatric evaluation, medication when appropriate, and therapies that address both conditions—resulting in better engagement, fewer relapses, and stronger overall functioning.
Conclusion
Freeing yourself from codependency and addiction opens the door to more stable recovery and healthier relationships. By understanding these dynamics and using evidence‑based treatments—individual therapy, family work, and peer support—you can reclaim autonomy and improve well‑being. Take the next step by reaching out for professional guidance tailored to your situation. Explore our resources and support options today to begin a practical, compassionate path toward lasting change.
**
